Borderline Personality Disorder - Symptoms and Treatment
Psychotherapy is the main treatment for this disorder. Treatment should be based on the needs of the patient rather than on the standards of the established diagnosis. Medications are useful in treating comorbidities such as anxiety disorders or depression. Short-term hospitalization has not been shown to be effective compared with outpatient psychotherapy and direct socialization assistance.
Long-term psychotherapy is currently the treatment of choice for BPD. Below are several methods, arranged in order of decreasing degree of understanding of their effect on the course of the disorder.[24]
- Dialectical Behavioral Therapy (DBT)[25]
The treatment period is one year or more. DBT is an adaptation of cognitive and behavioral psychotherapy methods aimed at reducing the symptoms of BPD, including suicidal behavior and parasuicides. The main therapeutic factor in this approach is the need to accept patients as they are, while at the same time encouraging them to make internal changes and teaching specific behaviors.
Acceptance into DBT is based on acceptance by the clinician, with further clarification of the patient's current emotions, judgments and behavior. This is called validation.
Whatever the form of validation, the patient always understands its content the same: “your thoughts and feelings are acceptable, you have the right to them.” Patients are actively taught emotional regulation, social effectiveness, stress management skills, goal setting, and self-control.
- SET-UP (Support, Empathy, Truth, Understanding, and Perseverance)[26]
The SET-UP system developed as a structured framework for psychotherapeutic work with borderline patients in times of crisis. At such moments, communication with them is significantly hampered by three main emotional states: melancholy and anxious loneliness, a feeling of separation and misunderstanding by others, an overwhelming idea of one’s own inadequacy.
The acronym “SET” translates to “Support, Empathy, Truth” and refers to a communication system consisting of these three parts. And the abbreviation “UP” stands for “understanding and perseverance” and indicates the goals that all participants in communication strive to achieve.
A statement representing Truth or Reality emphasizes that the borderline person is responsible for his or her own life and that attempts by others to help cannot replace that responsibility. The truth recognizes the existing problems and turns to the practical and objective side: “How to solve it?”, “What will you do about it?”
- based treatment (MBT)[27]
MVT is a structured treatment. In this approach, the total duration of treatment (12-18 months) and the timing of each session are clearly indicated. MBT is conducted in individual and group formats. The goal of the intervention is to increase the level of meaningfulness of one’s own actions, emotions, needs and life goals. The so-called “cognitive confusion” is overcome.
- Schema therapy
The effectiveness of this method has been confirmed by American psychologist Jeffrey Young.[28]
Schema therapy is based on several areas of psychotherapy: cognitive behavioral therapy, psychoanalysis, object relations theory, attachment theory, gestalt therapy. The core of schema therapy methodology is working with so-called early maladaptive schemas (EDS). RDS is a way of perceiving reality that was formed in childhood under the influence of traumatic events or abuse and is activated throughout life if there is some similarity of circumstances with childhood events.
Schema therapy aims to help the patient identify their schemas, recognize the source of the emotions that arise when the schema is activated, experience those emotions, and find ways to respond differently to events that activate the schema.
- Transference-Focused Psychotherapy (TFP)[29]
The method is based on O. Kernberg’s model of object relations for borderline personality disorder. TFP is a form of guided psychodynamic psychotherapy specifically designed for the treatment of BPD.
Transference interpretation is a key aspect of therapy and therapeutic change, but it is one of many treatment elements of this approach.
- Pharmacotherapy
A 2010 systematic review by Cochrane, an international organization that studies the effectiveness of health technologies, found that there are no medications effective for treating the core symptoms of BPD, such as feelings of chronic emotional devastation, identity disorders, and abandonment (loneliness).
However, the authors of the above review found that some medications may have an isolated effect on the symptoms associated with BPD. Haloperidol has been shown to relieve attacks of aggression, and Flupenthixol reduces the likelihood of suicidal behavior. One study found that Aripiprazole may reduce relationship problems and impulsivity.
Valproic acid salts can reduce (weaken) symptoms of depression, interpersonal problems and anger. Lamotrigine reduces impulsivity and anger.
Of the antidepressants, only Amitriptyline has proven its effectiveness. Additionally, omega-3 fatty acids have been surprisingly found to reduce depression and suicidal tendencies.[24]
Causes of BPD
Borderline personality disorder develops due to exposure to a number of external factors that cannot be controlled by the person.
- Heredity.
If the parents had this diagnosis, then the chances of it being diagnosed to the child in adolescence are quite high. Women suffer from this disease more often than men.
- Character traits.
If a person has low self-esteem, he is a pessimist by nature, his psyche is not resistant to stressful situations, he has increased anxiety, and the risk of developing borderline disorder is high.
- All forms of violence.
If a child suffered from emotional, sexual or physical abuse as a child, he or she may develop this disorder later in life. This also includes separation from one of the parents or their physical loss.
- Lack of emotional contact with a significant person.
Lack of attention on the part of the parent, his emotional coldness, and a subconscious prohibition on expressing his feelings lead to mental disorders. A similar picture is observed if significant adults expressed excessive or contradictory demands on the child. Unfavorable living conditions form a maladaptive pattern of behavior that manifests itself at a late age.
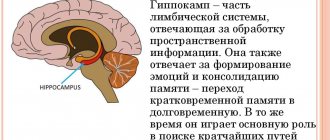
- Excessive activity of the limbic system of the brain.
This pathology occurs as a result of emotional deprivation, being a secondary disorder.
Nonspecific weaknesses in functioning
Borderlines have great difficulty coping with frustration and anxiety. In Kernberg's system, impulsive behavior is an attempt to relieve this tension. Borderline individuals also resort to defective tools of sublimation. This means that they are not able to channel frustration and discomfort into socially adapted channels.
Although people with BPD can display exceptional empathy, warmth, and guilt, these displays are often purely mechanical, manipulative gestures designed to create the appearance of feeling rather than express true emotion. Indeed, the borderline may act as if he had completely forgotten about the drama that erupted just a minute ago, just like a child who suddenly ends a tantrum with smiles and laughter.
Changing sense of reality
Like neurotics, people with borderline organizations remain in touch with reality most of the time. However, under stress, the borderline personality may briefly regress to a psychotic state.
Example: Marjorie, 29, sought therapy because of increasing depression and troubled family life. Being an intelligent, attractive woman, Marjorie responded calmly to everything during the first eight sessions. She readily agreed to a joint interview with her husband, but during the session she became uncharacteristically loud and combative. Having lost her mask of self-control, she began to vilify her husband for his alleged infidelities. She accused the therapist of taking her husband's side (“You men always stick together!”) and the two allegedly conspired against her. The sudden transformation from a relaxed, mildly depressed woman to a raging paranoid person is quite typical of the inherent ability of borderline personalities to quickly change the boundaries of reality.
Diagnosis of BPD
Diagnostics is the first and main stage before prescribing a course of therapy. The specialist takes the following steps step by step:
- a detailed survey of relatives, work colleagues and friends, which helps to establish the exact time when signs of borderline personality disorder first appeared;
- studying family history - it is important to make sure that close relatives do not have similar diseases;
- collecting maximum information about the patient’s life;
- conversation with the patient and observation of him from the outside in order to identify characteristic symptoms of mental pathology;
- conducting psychological testing to obtain a complete picture of the internal state of a mentally ill person.
Primitive thinking
People with borderline organization may perform well in structured work or professional environments. But beneath the shiny surface, there are usually serious self-doubts, suspicions and fears. The internal thought process of such a person can be surprisingly artless and simple, masking behind a stable façade of memorized and rehearsed platitudes. Any circumstance that penetrates the borderline personality's defense structure can unleash a flood of chaotic emotions. Marjorie's example (above) illustrates this point perfectly.
Projection psychological tests also reveal the primitive thought processes of people with BPD. These tests—such as the Rorschach and the Thematic Apperception Test (TAT)—provoke associations with ambiguous stimuli, such as inkblots or pictures, around which the patient builds a story. Borderline reactions usually resemble those of schizophrenics or other psychotic patients. While neurotic patients are more likely to give coherent, organized responses, BPD patients often describe bizarre, primitive images—they may see evil animals devouring each other where neurotics see a butterfly.
Types of disorder
Anxious personality disorder
There are several types of BPD:
- The low-functioning borderline personality is the most striking example of a disorder that is characterized by:
- frequent mood swings;
- the desire to tell everyone the “truth”;
- severe depression and suicidal tendencies;
- the presence of various kinds of dependencies;
- quarrelsomeness and a tendency to hooligan antics.
- High-functioning borderline personality type is a less severe stage of the disease, in which the patient can perform professional and social functions. Mood swings, quarrelsomeness and quarrelsomeness are perceived as individual character traits.
- An extroverted borderline personality - the patient constantly splashes out a stormy fountain of emotions on those around him, reflecting the individual’s attitude to the events that have occurred, and craves the approval and sympathy of society.
- Introverted borderline personality - all emotions accumulate inside the person, personal experiences do not manifest themselves to the people around them. Hiding the turbulent emotional inner world, the patient feels devastation and loneliness. Unhealthy suspiciousness sees the imaginary ill will and evil of the people around us. This type of disease often leads to suicidal behavior, completely unexpected for those close to them.
- The transparent borderline personality has a high degree of emotional control. Most often, in a professional setting, this is a nice, slightly narcissistic person, but all the accumulated negativity intensively spills out onto those closest to him, most often his family.
Important! BPD is not easy to define because many of its symptoms are not considered abnormal by society.