Borderline Personality Disorder (abbreviated as BPD
) is a rather rare mental destruction, characteristic of only 2-3% of people around the world. The pathogenesis of this type of psychopathy is usually accompanied by the presence of a complex of unfavorable factors.
It is quite difficult to recognize this type of disease in everyday life. Often, it is confused with narcissism or simply the bad character of an individual, since the behavior of “border guards” can be characterized by an extreme degree of unpredictability and hysteria, as well as a tendency to manipulation. For example, they confess their love to their partner, and after a couple of hours they leave “forever”; they can sincerely sympathize with someone, and then hit. It is also very common for patients of this type to constantly violate the boundaries of other people, shifting their problems onto them and avoiding responsibility. Let's look at the symptoms of borderline in more detail.
Symptoms of borderline personality disorder (BPD)
The main symptomatic difference of this type of disorder is the patient’s prolonged abnormal behavior
.
While in many other psychopathy periods of instability alternate with remission, in the case of BPD the patient behaves destructively over a long period of time. The field of psychological anomalies includes such manifestations as:
- aggressive behavior leading to relationship problems,
- unstable emotional background and inadequate self-image,
- high anxiety,
- total fear of loneliness and permanent feeling of boredom,
- dichotomous thinking and changeable moods, dividing the world only into “black and white” (today I love, and tomorrow I hate).
Also among the main symptoms can be noted: sociopathy and fear of society, associated with low self-esteem and, as a consequence, separation anxiety (an individual experiences it when separated from home or loved ones). Often, patients exhibit reckless, irresponsible “risky” behavior, the extreme form of which can be self-harm or suicide attempt.
Types of spontaneous actions accompanying mental borderline personality disorders
Due to difficulties in self-identification, lack of personal opinion, and a tendency toward polarity, BPD sufferers are prone to spontaneous destructive behavior.
A panicky fear of loneliness and the lack of an inner core pushes them into connections with sociopathic personalities who are characterized by destructive behavior: gambling, theft, vandalism, promiscuous relationships, drug addiction. This also includes self-harm, which was mentioned above.
One of the reasons for such uncontrolled behavior is the problem of maintaining internal impulse. The level of impulsivity is so high that a person is unable to control it.
How to help yourself or a loved one at home
What is borderline personality disorder Photo: Depositphotos
In short, the essence of home help comes down to three things:
- Calm down;
- Learn to control your impulse;
- To communicate with people.
Let's look at how to implement this in practice.
Tip 1. How to reduce emotional intensity
A person with BPD has low self-esteem. He seems to feel guilty for what happened to him in childhood and is happening now. Therefore, he is afraid that others will find out who he really is. In such a situation, it is important not to suppress your feelings and emotions, but to experience them without judgment or evaluation:
- Observe the emotions, as if from the outside - imagine that these are waves that come and roll back;
- Focus on physical sensations during emotions;
- Accept all your sensations;
- Realize that as soon as you allow yourself these feelings, they will no longer be so acute.
The second exercise that will allow you to quickly calm down is to influence your senses. Use different strategies in different emotional states.
- If you feel depressed, indifferent, lethargic, rinse your hands with cold or warm water, hold a piece of ice or squeeze any object, the edge of furniture, as tightly as possible.
- If you need to calm down, take a hot bath or shower, hug your pet, or wrap yourself in a blanket.
- If you feel empty, slowly eat a mint candy or a dish with an intense smell and taste - for example, something salty or spicy. If you need to calm down, drink hot mint tea or eat hot soup.
- Aromatherapy effectively helps bring emotions back to normal. Use scented candles, your favorite perfume, citrus fruits, spices, incense. Smell the flowers.
- Focus on a picture or photograph that catches your attention. Admire the beautiful landscape outside your window or simply imagine a place where you would like to be.
- Sounds will help you get rid of depression. Turn on loud music and blow a whistle. If, on the contrary, you need to calm down, listen to the sounds of nature: the sea surf, the sound of the forest, the singing of birds - all this can be easily found on the Internet.
Not everyone responds to sensory sensations the same way. Therefore, you need to try different options and determine the most effective ones for yourself.
With borderline personality disorder, any situation can trigger negative emotions. To minimize negative factors, try to follow simple rules:
- Get enough sleep;
- Exercise;
- Balance your diet - your diet should contain complex carbohydrates, proteins and fats in the correct proportions. And as little sweets, fast food, sweet carbonated drinks and processed foods as possible;
- Learn to meditate to relax.
Tip 2. How to control your impulse
Impulsivity occurs when heavy thoughts take over. To escape from mental pain, a person causes himself physical pain or goes into extreme sports - dangerous driving, casual sex, drunkenness. He feels better for a short time, but does not solve the problem globally.
As an ambulance, we recommend several techniques that will help you quickly relieve stress - and this is the first step to learning to control your emotions.
- Find a quiet, private place and sit comfortably. Focus on the sensations in your body - feel your arms, legs. Take a few deep breaths in and out. Watch your breathing carefully. After some time, the stress begins to release.
- Take a deep breath, fill your lungs to capacity with air and exhale in a slow stream. Repeat ten times.
- After inhaling and exhaling deeply, hold your breath. Count to twenty. After this, try to hold on for a few more seconds. And when you are already at the limit, start inhaling in a thin stream and imagine how the air gradually fills you. Repeat the exercise three to four times. Its essence is to switch the brain from emotional experiences to physiology - when there is not enough air, the body must save itself.
- After breathing exercises, consolidate the result with sensory sensations: listen to your favorite music, smell soothing aromas, hug a cat or dog. An interesting movie, workout, or walk will help you calm down faster.
Tip 3. How to consolidate your results through communication
Communication is the third key to helping with borderline personality disorder. And it needs to be used in conjunction with the first two – reducing the intensity of emotions and controlling impulses.
It is important that a person with BPD communicates with those he trusts - talks about his old and new feelings. About what has changed after performing techniques and meditations. This method helps you quickly escape from difficult thoughts.
Pathogenesis of BPD
The pathogenesis of the disease lies in incorrect or incompletely formed intrapersonal awareness of oneself, in other words, “self-identification.” Borderlines have difficulty understanding how they relate to major areas of life. They have problems with the concept of their opinions, interests, hobbies and their character as well. This is where the more common definition of the disorder – “borderline” – came from. In this aspect, it means maneuvering on the line between psychopathy and a stable state. The word “borderline” in this particular case means a precarious state between the norm and deviation, as if a person lives on the border between “mental illness” (psychosis) and “mental health”. That is why the slang name for patients of this type is “borderliners” (from the English expression “border line”, which literally translates as “border”).
In classical psychiatry, borderline personality disorder is also classified as a type of ego-syntonic disorder. Ego-syntonicity implies that the patient does not evaluate his condition as painful, is not critical of it, and calmly accepts deviations in behavior, without considering that they harm him in any way. Moreover, the patient seems to “defend” his symptom, preventing his own healing due to the difficulty in identifying his own “I”.
Questions and answers
Can borderline disorder be treated at home?
No. Such mental disorders are treated in a hospital setting. The patient can cause physical harm to the life and health of others, as well as to himself. Therefore, he needs hospitalization.
Is it possible to get rid of BPD using folk remedies?
No, using questionable drugs will only worsen the situation. Any medications are used after prior consultation with a doctor.
Causes of BPD
The underlying causes of borderline disorder are not clearly defined at this time, however, like most other disorders, BPD is caused by a group of factors.
Hereditary (genetic determination), physiological (impaired brain function) and social factors (low resistance to stress and psychological traumatic factors).
Unfavorable social environment
According to statistics, groups of people exposed to an unfavorable social environment, for example in the family, are more often susceptible to the disease. This may include:
- difficult childhood
- abuse,
- tyranny
- physical or emotional violence in the family,
- early loss of parents.
It is worth noting that among women “borderline” is 3 times more common than among men.
Post-traumatic stress disorder (PTSD)
, as a variation of an unfavorable social factor, can act not only as a cause, but also as a concomitant separate disease that is in a pathogenetic relationship with the diagnosis in question.
Chronic childhood emotional trauma may contribute to the development of BPD, but in rare cases it is the sole cause. Personal qualities responsible for the ability to cope with a stressful situation in this aspect also play a big role. It is worth noting here that, according to statistics, trauma received in childhood (especially before the age of 10) is much more likely to lead to subsequent disorder than that received in adulthood. Scientists also note that situations not associated with direct violence, such as natural disasters or catastrophes, are less likely to lead to the development of post-traumatic syndrome.
Physiology
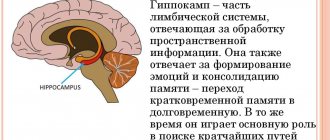
Another group of factors considers a possible cause of the development of the disease - disturbances in the functioning of neural brain connections, namely the destruction of the functioning of frontal-limbic neurons
Heredity
The third significant cause of BPD is genetic predisposition, which accounts for up to 40% of cases of this diagnosis. It is quite difficult to achieve clear indicators in this regard, however, according to European studies, BPD is ranked 3rd out of 10 in terms of genetic determinants among personality disorders. It is logical to note that deviations in the functioning of certain lobes of the brain can be inherited and lead to a number of psychological problems, the development of which is aggravated by social factors. Most studies show that borderline personality is most often inherited from the mother.
Borderline mental state in psychiatry and severity of personality disorders
In clinical psychiatry, three levels of mental disorder are traditionally distinguished:
- Neurotic
. This includes neuroses of various types, implying reversible temporary conditions that can be treated. - Psychopathic
level. In its plane lie personality disorders, which include character anomalies of various pathogenesis or painful changes in his traits, with which nothing can be done, since they relate to the personal structure of the individual. - And finally, the deepest damage to the psyche manifests itself at the psychotic
level. This includes manifestations such as delusions, hallucinations, and twilight consciousness.
In modern psychoanalysis, there are 4 levels of deviations. Between the state of psychosis and neurosis the “ borderline”
level", also called
borderline state
. A borderline state can mean both the disorder itself and a designation of the level of mental damage.
Symptoms
Such conditions may present differently depending on the type of disorder. Among the main signs are
- frequent feelings of anger, anxiety, danger, worthlessness;
- feeling of emptiness;
- avoidance of communication with people;
- the appearance of irritability, even if the stimulus is minimal;
- frequent conflicts with others, which may be accompanied by insults, death threats, and physical violence;
- a feeling close to the feeling of losing contact with reality;
- great difficulties in maintaining normal relationships with loved ones, or the impossibility of this.
How to Reliably Identify Borderline Personality Disorder (BPD)
Borderline personality disorder is extremely difficult to diagnose and differentiate, as it has a high level of comorbidity, in other words, it is combined with a large number of concomitant disorders. For example, panic anxiety, eating disorder, bipolar affective disorder, attention deficit disorder, sociopathy, and so on. Due to the above, the patient has to undergo a lengthy diagnostic process and special tests.
Test for borderline personality disorder BPD
One of the fairly popular tools for identifying the presence of psychopathy are tests, which are essentially a personality questionnaire. The test used in modern clinical psychology to screen for strong signs of BPD was developed in 2012 by a group of scientists. In their work, the authors relied on the basic criteria for differentiating borderline disorder.
The questionnaire edited by them is a fairly effective tool for diagnostic verification and confirmation of symptoms. It is used both in psychiatric and general clinical settings, as well as in other practices that are not directly related to medicine.
The test itself consists of 20 questions and asks the test taker to answer only yes or no. For each answer, the system counts a certain number of points. The likelihood of diagnosing BPD appears if the respondent scores more than 25 points.
Classification of mental disorders
First, it is helpful to understand the basic terms used to describe disorders. Depending on the nature, source of origin:
- Endogenous. The reason is metabolic disorders, malfunctions of the endocrine system, hormonal imbalances, genetic predisposition, etc. The main problem is that at this stage of medical development it is impossible to establish an unambiguous connection between processes in the body and the development of such disorders. And the processes themselves cannot always be identified or even suspected.
- Somatogenic. A type of exogenous psychopathology. The cause is a specific physical (somatic, bodily, carnal) disease, due to which metabolism, blood supply to the brain, hormonal levels, etc. are disrupted. The difference from endogenous ones is that the specific disease-cause is precisely known, and the connection between it and a mental disorder is clearly established.
- Psychogenic. A type of exogenous psychopathology. The reason is a severe reaction of the psyche to negative events in life: prolonged stress, illness or death of a loved one, financial difficulties, lack of demand in the profession, in personal life, etc. Initially, there are no physical prerequisites for such disorders, their source is external, in society, surrounded.
Separately, we note mental disorders that develop as a result of addictions (alcoholism, drug addiction, etc.). This is a special case of somatogenic disorders, but very specific, so it is usually considered separately.
Depending on the nature of the pathological manifestations, psychopathologies are distinguished:
- Non-psychotic. Such manifestations may well occur in completely healthy people with, for example, severe fatigue. Only in healthy people they will not be as strong and lasting. Non-psychotic disorders are characterized by maintaining a generally adequate perception of reality and maintaining a connection with it. Non-psychotic disorders are most often psychogenic.
- Psychotic. By definition, such manifestations do not occur in healthy people. These are disturbances of consciousness, thinking, and perception, in which an adequate understanding of reality is lost and communication with it is lost. For example, wild mood swings, hallucinations, delusions, disorganization of cognitive functions. Psychotic disorders are often endogenous or somatogenic.
Some diseases, for example, psychogenic (neurotic) depression, can, with an unfavorable course, move from non-psychotic manifestations to psychotic ones. Delirium of self-deprecation develops, the mood is extremely depressed, reality is perceived exclusively through the prism of a depressive picture of the world. But in general, most pathologies remain within their original group.
The structure of the human brain. The brain, together with the spinal cord, makes up the central nervous system. Its lesions in most cases lead to mental disorders. And mental disorders in one way or another affect the central nervous system and higher nervous activity.
The current Schedule of Diseases is very far from perfect. But, oddly enough, the section devoted to mental disorders is organized surprisingly conveniently, competently and logically. The fifth chapter includes seven articles, from 14 to 20. Each article is devoted to examination for diseases of a particular group. Briefly about each.
Organic mental disorders – Article 14
These are any mental disorders caused by any brain damage. Infection (neurosyphilis, meningitis, encephalitis), any inflammation, tumors, injuries, impaired blood supply to the brain due to damaged blood vessels - it doesn’t matter. The degree of impairment ranges from mild behavioral changes to, for example, dementia and other cognitive disorders of varying severity. The inspection options are as follows:
- Category “B” (suitable with minor restrictions, subcategory “B4”) - with stable compensation of manifestations that developed as a result of ONLY two conditions: either an acute disease (infectious) or a closed craniocerebral injury. Open TBI or tumor excludes category B.
- Category “B” (limited suitability) – for moderate mental disorders. The criteria for moderation are not specified, but in practice this means any illness, except those that give category “B”, if they do not lead to disability of the young person. For example, mild mental disorders due to closed TBI.
- Category “D” (unfit) – for severe and persistent mental disorders. This actually means disability, perhaps even with incapacity. For example, dementia due to the death of areas of the cerebral cortex or hallucinosis caused by metabolic disorders in the brain.
In case of temporary and completely passing disorders (for example, after an injury or head wound), the category “G” (temporarily unfit) is placed for the period of treatment and recovery. It provides a deferment for health reasons for a maximum of a year, after this period they must be recognized as either fit (“B”) or unfit (“C” or “D”), but in the second case they can actually put “G” again for a year so that Don't write off the conscript at all. This is not correct, it is better to achieve a permanent unfit category.
Endogenous psychoses – article 15
They traditionally include two groups: schizophrenia spectrum disorders and affective psychotic disorders. The first group combines schizophrenia, schizotypal, schizoaffective, schizophrenomorphic (schizophrenia-like) disorders. The second includes mania and endogenous depression in various combinations (for example, bipolar affective disorder), as well as dysthymia and cyclothymia. In any case, examination for any diagnosis in this group is only category “D” (unfit), without options. The article has no notes, comments or explanations - there are literally two or three such articles in the entire Schedule.
Somatogenic disorders – Article 16
The schedule defines them as “symptomatic and other mental disorders of exogenous etiology” and includes any mental disorders due to any infections and somatic diseases except those that directly affect the brain, as well as poisonings (intoxications), except those caused by addictions. Inspection in the following categories:
- “B” (subcategory “B4”) – with a mild and short-term course (no more than two to three weeks), only with non-psychotic symptoms, with complete recovery.
- “B” – with moderate manifestations, with repeated cases (relapses) lasting more than three months, including damage to the central nervous system or pathological changes in personality due to organ damage. Symptoms may be non-psychotic or mildly psychotic.
- “D” – with pronounced manifestations, with a long course, with strong pathological changes in personality. This category is assigned to disorders of the psychotic type, that is, with delusions, hallucinations, disorganization of the intellectual sphere, loss of a realistic perception of the world, etc.
In case of minor or moderate manifestations for no more than three months, they are placed in category “G” with a deferment from conscription for six months or a year. In this case, in any case, the specific somatic disease that led to the mental disorder and the connection between this disease and this disorder must be established.
Neuroses and related disorders – Article 17
This is the largest category. About half of all visits to psychiatrists are related to disorders of this group. The article combines the following classes of psychopathologies:
- Neuroses proper (neurotic disorders) - neurasthenia, hysterical neurosis, obsessive-phobic neuroses (social phobia, obsessive-compulsive, generalized anxiety, panic and other disorders).
- Dissociative (conversion) disorders - also caused by a severe reaction to stress, but manifesting deeper than classical neuroses. This is dissociative amnesia, identity disorder (split personality), etc.
- Somatoform disorders - their causes are the same as those of neuroses, but the manifestations are exclusively somatic, in the form of causeless pain in different organs and parts of the body (heart - cardioneurosis, stomach - gastroneurosis, etc.).
The Schedule also includes psychogenic depression, psychogenic psychoses (for example, reactive depression, hysterical psychosis), personality changes after reactive states, as well as a neurotic type of personality development (roughly speaking, a constant background undifferentiated neurosis). The examination is carried out in categories “D”, “B” and “B” (subcategory “B4”). Read more in a separate article on neuroses.
Personality disorders - Article 18
The article brings together all disorders associated with behavior, preferences, habits and current mental development. Let's briefly list the categories:
- Personality disorders themselves (in the old sense psychopathy) are pathological forms of personality with a disturbed emotional sphere, often with a predominance of the intellectual sphere over it: epileptoid (impulsive), schizoid, paranoid, hysterical, borderline, anxious, avoidant, etc.
- Disorders of habits and drives: gambling addiction (compulsive gambling), pyromania (arson), kleptomania (theft), trichotillomania (hair pulling in instinctive attempts to relieve anxiety and restlessness).
- Gender identity disorders (transvestism, dual role transsexualism, childhood gender identity disorder) - that is, an obsessive desire to live and appear to others as a member of the other sex without a real intention to change it surgically and documented.
- Disorders of sexual preference: fetishism, voyeurism, exhibitionism, sadomasochism, pedophilia, bestiality, necrophilia, etc. These are associated with behavioral disorders associated with rejection of one’s own sexual orientation. “At the same time, sexual orientation in itself is not considered a disorder,” including homosexual and bisexual.
- Childhood emotional and behavioral disorders that persisted at the time of conscription, for example, attention deficit hyperactivity disorder (ADHD), some forms of antisocial, deviant behavior of young people.
- Disorders of psychological development that appear in adulthood (after the end of puberty), including eating disorders (anorexia and bulimia).
Examination only for non-conscription categories. Roughly speaking, the very fact of the presence of a disorder already means category “B”, even if it is expressed moderately and is somehow (unsustainably) compensated. With more serious severity - category “D”. It is important that the personality as a whole has a pathological structure - individual manifestations similar to symptoms do not mean that the conscript has such a disorder.
Addictions and disorders resulting from them – Article 19
This includes alcohol, drug and toxic addictions - respectively, chronic alcoholism, drug addiction, substance abuse. Alcohol, drugs and toxic mixtures are collectively called psychoactive substances. Consequences - alcoholic psychoses (for example, delirium, hallucinosis or alcoholic dementia), behavioral disorders, pathological personality changes, depression of memory, thinking, etc.
Examination is carried out only for non-conscription categories. For minor violations or “clearly harmful consequences,” including delirium tremens (delirium tremens), category “B” is assigned; for moderate and severe ones, including chronic alcoholic psychoses, category “D.” Fortunately, for men of military age this article is now of little relevance, because the “lucky” owner of category “D” is most likely no longer able to realize his “happiness”. But perhaps fortunately.
Mental retardation – Article 20
In the last century, it was officially called oligophrenia - literally feeble-mindedness, dementia. Based on intelligence quotient (IQ), three levels of mental retardation were distinguished:
- debility (from 69 to 50 points, the level of mental development approximately corresponds to a child 9-12 years old) – socialization and simple work are possible;
- imbecility (from 50 to 20 points, like a child 3-9 years old) – work is practically excluded, socialization is not always possible and with restrictions;
- idiocy (below 20 points, like a child under three years old) - a complete lack of ability for independent household services.
Nowadays the more correct term “mental retardation” is used; four levels are distinguished:
- light (corresponds to debility);
- moderate (from 50 to 35 points, like a child 6-9 years old, work is practically excluded, socialization is limited);
- severe (from 35 to 20 points, like a child 3-6 years old, socialization is extremely limited or completely impossible, there may be basic household self-care skills such as maintaining personal hygiene);
- deep (corresponds to idiocy).
Evgeniy Godov
lawyer
Medical examination covers only non-conscription categories. If the degree is mild (moronic) they put “B”, for the rest – “D”. The main criterion is clinical diagnosis and psychological testing for intelligence, not always in an inpatient setting. They are mandatory for borderline, ambiguous cases.
Ask a Question