The main symptoms of delirium tremens are auditory, visual and tactile hallucinations. It seems to the patient that insects are crawling on him, that there is someone in the apartment besides him and his household members. He becomes paranoid and even aggressive towards loved ones.
Emergency care for alcoholic tremens includes calling an ambulance and visiting a narcologist. This must be done urgently, because delirium can cause serious harm to both the addict and his family members.
How to recognize delirium tremens?
The symptoms of delirium tremens are described in the Latin name for this disease: delirium tremens, which literally means “shaking darkness.” The two main signs of psychosis are: clouding of mind and trembling of the whole body.
Among narcologists, it is customary to divide fever into three stages. Symptoms appear 2–3 days after quitting binge drinking and gradually increase over the course of a week. Most addicts come out of delirium tremens acutely, falling into a long, deep sleep, but some can come out of it gradually.
In the first, the patient suffers from mood swings. He experiences anxiety, which gives way to a state close to euphoria. Anxiety attacks become longer, hand tremors are observed, and the rate of speech accelerates. The person looks either pale and anxious, or unnaturally joyful.
At the second stage, hallucinations occur. They begin at the moment of falling asleep, giving way to nightmares. A person is unable to separate nightmares and reality, which is why even after waking up he sees insects, monsters, maniacs, strangers and animals, and mythical creatures. Some alcoholics feel that their relatives want to harm them, while others, on the contrary, try to protect their loved ones from an imaginary danger. Over time, insomnia comes, but the intensity of hallucinations only increases.
The third phase is the exit from psychosis. Most often, a person comes out of delirium quite abruptly, falling into a long sleep. Subsequently, the patient feels tired, hypomanic or depressed. Typically, an alcohol addict remembers hallucinations well, but has difficulty telling what was a figment of his imagination and what actually happened.
Development of withdrawal syndrome
Withdrawal syndrome may appear within a few hours after the last drink. The main stages and possible complications are listed below. Please keep in mind that these are general cases and there may be exceptions.
Withdrawal symptoms can be deadly.
The first stage of withdrawal involves the onset of minor symptoms, usually subsiding in less than 12 hours after the last drink. These include anxiety, insomnia, nausea, headaches, loss of appetite, sweating, and fast or irregular heartbeat.
12 to 24 hours
During this period of time, tactile, auditory, or visual hallucinations may occur . Visual hallucinations are the most common. For example, a person may see something dangerous outside the window, break the glass and cut himself. The patient may experience a burning sensation, itching or numbness that has no physical cause.
24 to 48 hours
Severe withdrawal attacks most often occur during this period. This can be very dangerous as life-threatening complications can occur. Typically, most symptoms resolve within a maximum of five days , but full recovery may take weeks.
Why does delirium delirium occur?
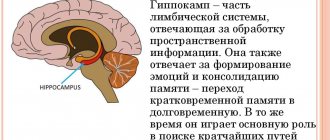
The main cause of psychosis is brain damage caused by toxin poisoning. Most often, men over forty with a long history of alcohol addiction, who are prone to binge drinking, suffer from the problem. During this time, the body undergoes serious changes in metabolic processes, literally rebuilding itself, adapting to the regular intake of ethanol. As soon as use stops, withdrawal symptoms begin—alcohol withdrawal. An organism that has adapted to alcohol experiences severe stress, which leads to psychosis, “shaking darkness,” a phenomenon that equally affects the psyche and physiology.
Sometimes the causes of delirium are previous infections, sometimes - traumatic brain injuries. But against the background of alcoholic psychosis, these cases are relatively few in number.
Literature:
- Alcoholic delirium and delirious-oneiric psychoses of complex structure / K.G. Danielyan. - Yerevan: Hayastan, 1977. - 132 p.
- Alcoholic psychoses: (clinic, pathomorphosis, therapy) / A. V. Pogosov, K. A. Kurzhupov; State higher educational institution prof. education "Kursk State. honey. University" Ministry of Health and Social Development of the Russian Federation. - Kursk: Kursk State Publishing House. honey. University, 2011. - 224 p.
- Acute alcoholic psychoses [Text] / M. G. Gulyamov, E. T. Grigoryants, B. Ya. Rakhminov. - Tashkent: Medicine, 1975. - 121 p.
Why is delirium tremens dangerous?
The consequences of fever are terrible - these include mental disorders, neurological pathologies, metabolic disorders, and severe damage to the liver and kidneys. A person suffering from cardiovascular disease may simply not survive prolonged and painful delirium, which exhausts him physically and psychologically. Subsequently, all this requires long-term recovery and rehabilitation, most often the involvement of medical assistance.
Another danger of delirium is the risk that an alcohol addict, under the influence of hallucinations and paranoia, will harm loved ones. For example, alcoholic delusions of jealousy are quite common, when the patient - most often a man - begins to suspect his wife of infidelity. Usually, delusions of jealousy develop over some time: first, the addict suspects his wife of infidelity while drunk, then the delirium spreads to moments of hangover and even sobriety. Often the paranoia is frankly ridiculous, but the patient is completely convinced that he is right. During delirium, plausible hallucinations may join paranoia: the imagination pictures lovers right in the apartment.
It's easy to imagine what this might lead to. In such situations, wives, children, and innocent imaginary “lovers” often suffer.
Second stage
This period is called full-blown delirium - the complex of symptoms and conditions of the patient reaches its peak in its manifestation. The behavior of an alcoholic at this stage:
- sees the people around him as a threat to his life;
- aggressive;
- experiences auditory, tactile, visual hallucinations;
- perceives surrounding objects as animate;
- feels as if there is something in the mouth.
Discomfort in the oral cavity is associated only with mental distortion and slight swelling of the mucous membranes. During delirium, the patient feels as if he is about to suffocate, those around him want to kill him, and objects are animate, nightmarish creatures.
The first thing to do at this stage is to call an ambulance, describe in detail what is happening to the patient, and take him to a specialized narcology department as soon as possible.
How is delirium tremens treated?
As soon as a person jumps up in the middle of the night and begins to claim that there is someone in the apartment, you need to call an ambulance. Many Russians try to cope with delirium on their own, but it is difficult and dangerous. Before doctors arrive, the patient should be put to bed and given cold water. If he is aggressive, do not try to deal with him by force, try not to threaten or provoke him. If he is downright dangerous, go to the neighbors.
Recovery from binge drinking in a hospital setting includes the removal of ethanol breakdown products from the body, restoration of water-salt balance and support with various means: vitamins, minerals, hepatoprotectors. The patient receives sedation, which helps him recover from delirium with minimal damage.
Since psychosis can last more than a week, constant monitoring by specialists is more effective than detoxification at home.
Severe forms
The most dangerous types of delirium for alcoholics are:
- Professional
The patient experiences mental disorders not in the evening, as in most patients with withdrawal syndrome, but during the day. The person is silent, despite internal excitement, or speaks in rare spontaneous phrases.
The concept of “professional” is associated with monotonous movements , which are usually associated with his daily activities. He will monotonously repeat the movements that he often made before, washing dishes, driving a car, working on a computer.
After normalization of health, complete amnesia occurs.
- Mussitating
Occupational delirium is often replaced by the “muttering” form. Hallucinations are usually absent, but there is marked confusion of consciousness. The patient lies in bed, so attacks of excitement are limited to his position: he can make grasping movements and pronounce short syllables.
After regaining consciousness, the patient also does not remember what happened to him.
Severe forms can cause death, so the patient needs immediate medical attention.
Is it possible to provide first aid for delirium tremens?
Is it possible to help a person on your own - for example, until the drug treatment team arrives? If a person is aggressive and prone to attack, it is recommended to go to another apartment so as not to provoke him and not become a victim of an attack. If the hallucinations are rather harmless in nature, then you can try to provide first aid yourself:
- create a calm environment without unnecessary noise or loud appliances, draw the curtains, close the door;
- give plenty of drink, but in no case force it;
- put him to bed and apply cool compresses until the narcologists arrive.
You can give mild sedatives, but in general it is not advisable to provide medical treatment for delirium tremens without the presence of a doctor. A team of narcologists knows how to properly help a person in a state of delirium; they have all the drugs with them and a competent schedule for their administration. It's better to wait for them.
Signs and associated symptoms
Common signs of delirium tremens include nausea, vomiting, body tremors, high blood pressure, abnormal heartbeat (tachycardia), sensitivity to light and noise, intense feelings of anxiety, fear or paranoia, overexcitement, decreased alertness, visual or auditory hallucinations (very common). seeing, hearing or feeling things that are not there), disorientation, confusion and insomnia. These symptoms are dangerous both for the person experiencing them and for those around them.
How is recovery after delirium tremens?
Delirium tremens is an irreversible condition that causes significant harm to the body. The brain is especially affected: the result of the “squirrel” in some cases is temporary loss of speech, various types of paralysis, memory loss, and deterioration of cognitive functions. Against the background of fever, various mental illnesses and personality disorders develop. It becomes the starting point for many chronic ailments.
Recovery from delirium tremens depends on the degree of damage - brain, liver and kidneys, cardiovascular system. A psychiatrist-narcologist will prescribe therapeutic procedures, some medications designed to improve organ function and reduce alcohol “destruction,” and medications to improve cognitive abilities. In some cases, physical therapy and rehabilitation in various centers are required.
The older a person is and the longer his experience of alcoholism, the worse the consequences of fever. However, everyone has the opportunity to recover from addiction.
After the acute symptoms of fever are relieved, you can talk with the patient about help and recovery, treatment of alcoholism, and invite a narcologist to your home. Delirium often brings with it a temporary aversion to alcoholic drinks, which can be used as a good start in getting rid of addiction.
Content:
- Symptoms
- Duration
- First stage
- Second stage
- Threat to life
- Treatment methods and consequences
Delirium tremens, the symptoms of which resemble psychosis, is otherwise called delirium tremens. Vivid symptoms appear against the background of cessation of alcohol consumption in alcoholics in the second and third stages of addiction. The patient is not able to take responsibility for his actions, and therefore requires emergency medical care.
Harbingers
Even before the onset of the actual attack, during the hangover stage the following symptoms are observed:
- speech and hearing disorders;
- convulsive seizures (in every tenth patient);
- persistent insomnia or sleep disturbances that become superficial, with frequent abrupt awakenings, and do not give a feeling of rest;
- poor sleep begins to be accompanied by severe nightmares;
- a person feels an incomprehensible anxiety, he is tormented by a premonition of troubles and misfortune.
Physiological signs are expressed in:
- tremor;
- profuse sweating;
- tachycardia;
- temperature increase;
- increased blood pressure;
- severe redness of the skin on the face and retina of the eyes.
Even when a person is awake, he experiences various hallucinations in auditory and visual form: whispers and voices, incomprehensible steps, suspicious knocks and rustles.
Principles of treatment
Treatment only in a hospital, which includes:
- intravenous administration of vitamins, neurometabolic brain stimulants, magnesium and potassium, sedatives and hypnotics, special medications to maintain heart function;
- administration of large volumes of fluid;
- Constant monitoring of heart and kidney function.
Potent tranquilizers are prescribed only at night due to side effects.
This disease cannot be treated with psychotropic medications alone.
Currently, the patient is usually sent to a drug treatment or psychiatric department. The patient can be dangerous both for himself and for the people around him.