Everyone in their circle of friends has a person who constantly complains about their health: they have a stabbing pain, they are sick, or they simply don’t feel well. But no matter how many times he goes to doctors, no one finds a specific reason for this condition. He’s pretending, we think. But don't rush to conclusions. These symptoms may be a sign of a somatoform nervous system disorder. It does not have an organic background, but leads to a mental imbalance of the individual.
Why does the disorder develop?
Somatoform disorder is a disease of a psychological nature in which the symptoms of damage to internal organs are functional, not organic.
Such dysfunction is detected in 0.5% of the world's population, and it affects mainly women. The reason lies, first of all, in the psychological state of a person.
The first group of factors influencing the occurrence of the syndrome is heredity and character traits. For example, people with asthenoneurotic and hysterical types of character are more likely to develop it. They are characterized by hypersensitivity, timid or demonstrative behavior. Such people are characterized by rapid nervous exhaustion; as a rule, they are pessimistic.
The second group is psychogenic traumatic external influences. These include acute stress factors, when a powerful psychological blow at once leads to a disorder of nervous activity. This could be the loss of a loved one, a decrease in social status, or a situation of severe fear.
Chronic stress occurs as a result of systematic mental and physical overstrain, lack of positive emotions, unmet needs and excessive demands on oneself.
It is worth noting that somatoform disorder very often develops in people who are emotionally stingy, hide their feelings, and do not know how to express them. And since emotions need a way out in any case, they find it in this unique way. A similar state can accompany members of religious families, where an atmosphere of strict morality reigns.
Other factors that provoke the disorder include complicated pregnancy, trauma, infections, and some somatic diseases.
Treatment of somatoform disorder
Treatment of somatoform disorder is long-term and carried out comprehensively, combining drug treatment and psychotherapy. Psychotherapy helps the patient reconsider his beliefs and physical sensations, and learn to cope with stress and anxiety. Pharmacotherapy eliminates anxiety and corrects mood. Drugs are selected according to the clinical picture.
At the Re-Alt clinic, the method of psychotherapy is selected taking into account the form and severity of the somatoform disorder. Often used in treatment are cognitive-behavioral and dynamic therapy, training in relaxation skills, and group classes to improve communication and social skills.
Lack of timely treatment can lead to loss of performance, problems in social relationships, and the risk of developing concomitant mental disorders increases.
If you notice signs of somatoform disorder in yourself or your family, we will provide you with qualified assistance, of high quality and at an affordable price. Our clinic is located in the center of Moscow, on Vsevolozhsky Lane, next to the Kropotkinskaya metro station. The specialists at the Clinic of Dr. Shmilovich “Re-Alt” are interested in your speedy recovery.
Signs of illness
Symptoms of somatoform disorder are quite varied and manifest themselves in malfunctions of almost all body systems.
| System | Symptoms |
| Cardiovascular | Arrhythmias, sharp increases and decreases in blood pressure, pain and discomfort in the heart area. |
| Respiratory | Hyperventilation syndrome: shortness of breath, feeling of lack of air, dizziness. |
| Digestive | Irritable bowel syndrome: bloating, abdominal pain, diarrhea. Digestive disorders: poor appetite, nausea, vomiting, difficulty swallowing, feeling of a lump in the throat |
| urinary system | Frequent urination, pain when passing urine. |
| Genital area | Decreased libido, inability to achieve orgasm. Vaginismus in women; in men – weak erection, impaired ejaculation. |
| Other symptoms | Increased sweating of the palms and feet, chills, hyperthermia. |
As a rule, several symptoms associated with different systems occur simultaneously.
There are the following types of this disorder:
- hypochondriacal;
- somatized;
- somatoform dysfunction of the autonomic nervous system (SDVNS);
- chronic somatoform pain disorder;
- undifferentiated somatoform disorder.
Patients with somatoform dysfunction are distinguished by several features. This includes a peculiar, emotional or overly specific narrative about one’s condition. For example, a man comes to a cardiologist with pain and discomfort in his heart. But at the same time, he speaks not only about their character, but also about the fact that they cause him a lot of inconvenience. Such attacks occur at work, at the moment when he is supposed to make a report on his achievements. As a result, he cannot concentrate, paying all attention to his heart.
The reason here is this aspect: perhaps the man is psychologically not ready to talk about his work (for example, due to his failures), and the heart is assigned to the extreme. And it is precisely this that reacts to this stressor in order to divert attention from it.
Other distinguishing features are:
- exaggeration of pathological sensations;
- denial of the role of psychological factors in their development;
- increased irritability towards others.
Autonomic dystonia syndrome
Autonomic dystonia syndrome is all forms of disturbance of autonomic regulation, most often secondary manifestations of various pathologies.
There are 3 forms of SVD:
- psychovegetative – a feeling of tightness in the chest, changes in heartbeat, stomach pain, frequent vomiting, headache, dizziness, neuralgia of various locations, problems with urination, increased sweating, changes in the menstrual cycle, feeling cold;
- peripheral autonomic failure syndrome - (see autonomic failure);
- angiotrophalgic - vascular (marbling of the skin, redness, pallor, cyanosis, feeling of numbness, tingling), trophic (peeling and thinning of the skin, spots of pigmentation or depigmentation, ulcers, more often in the area of the hands and feet, brittle nails) and painful manifestations (paroxysmal prolonged pain , having a shooting, aching, burning, tingling, etc. character.
Hypochondriacal dysfunction
Hypochondriacal disorder is characterized by a person's extreme concern about his or her health. He is sure that he is developing a severe, sometimes fatal disease. But their types may vary from case to case. One time the patient thinks that he has cancer, another time it is a severe heart pathology, etc.
The degree of sensation also changes. Either it seems to the individual that he is on the verge of death, then the manifestations become quite bearable.
It has been established that about 14% of patients visiting doctors of various specialties suffer from hypochondria. Most often it occurs in childhood and adolescence, as well as in mature people.
Basically, the patient is accompanied by the following symptoms:
- from the cardiovascular system - pain in the heart, disruptions in its functioning. The patient's conclusion is heart defects, heart attack;
- from the digestive system - abdominal pain, diarrhea, constipation. Conclusion – stomach and intestinal cancer;
- on the part of the excretory system – fear of uncontrolled urination, and therefore patients even limit leaving the house. Pain in the lower abdomen.
Important criteria for recognizing pathology are the presence of senestopathies and mood disorders.
Senestopathies are manifested by unusual and painful tactile sensations. This may be itching and burning, a feeling of cold, compression and constriction, pulsation of blood in the vessels, twisting, displacement and other similar phenomena.
Mood disorders manifest themselves in increased anxiety, sadness, melancholy, and a feeling of hopelessness. Patients focus only on themselves, and do not hear others at all. At the same time, they believe that no one needs them, everyone has abandoned them.
Such people systematically seek help from doctors. And if a specific disease is not found, they insist on re-examination.
The following nuances will help determine pathology:
- constant belief that a person has a serious illness, often with other concomitant illnesses. And even numerous normal examination results cannot convince them;
- lack of trust in doctors, despite their regular visits;
- the activity of such a patient is not aimed at alleviating the condition, but at confirming the presence of a progressive pathology;
- constant concentration on your illness;
- independent diagnosis.
As hypochondria worsens, it can develop into a paranoid state or hypochondriacal depression.
The diagnosis of hypochondriacal disorder is made when schizophrenia and schizotypal disorders, bipolar affective disorder are excluded.
Hypochondriacs are often found among famous people. Actor and director Woody Allen is one of them. One day, his illness saved him from food poisoning. The entire crew ate pizza, which only he refused due to concerns about his health. As a result, everyone except him developed an eating disorder.
Modern clinical psychiatry, according to a number of researchers [170, 365, 411, 519], still does not have unambiguous recommendations for the treatment of somatoform disorders (SSD). Conducted by G. Andrews et al. [204] a survey of specialists showed significant differences in the opinions of psychiatrists about the role of psychotherapy and medication. Significant disagreements reflected in the literature boil down to the following two points of view. Some authors attach the greatest importance to various psychotherapeutic techniques [382, 436], others [204, 365, 411, 459, 529] emphasize that psychotherapy aimed at correcting pathopsychic processes, although it plays an important role, still cannot be considered as universal method of therapy and must be combined with medication.
The contribution of pharmacotherapy to the complex of treatment measures increases as psychopathological disorders become more severe and/or chronic. This provision applies to the treatment tactics of the main forms of SFR: asthenic [298, 470], dysmorphophobic [69, 360, 550], conversion [86, 145, 530], algopathic [330, 404, 529] disorders. However, the opinions of researchers differ in the choice of medications recommended for the treatment of FDS. While some authors [307, 310, 330, 360] prefer antidepressants, others [27, 102, 218, 295, 355, 483, 519] prefer tranquilizers, others [547] prefer carbamazepine, and others [86, 189] prefer neuroleptics.
Of particular importance from the point of view of the objectives of this work are those studies in which treatment recommendations are differentiated in accordance with the clinical characteristics of SFR.
Moving on to the analysis of these publications, we will focus primarily on those devoted to the treatment of asthenic conditions. The traditional approach to the treatment of asthenia is based on a typology that involves distinguishing hypersthenia and hyposthenia. Thus, G. Ya. Avrutsky and A. A. Neduva [3] indicate that if hyperesthetic manifestations predominate in the clinical picture of asthenia, treatment is based on “inhibitory” tranquilizers, to which the authors include meprobamate, nozepam, phenazepam; for hyposthenia, tranquilizers “with a stimulating component” are indicated - trioxazine, mezapam, sibazon. Drugs of this class, according to A. M. Svyadoshch [141], M. E. Teleshevskaya [176], are advisable to combine with psychostimulants or nootropics, and nootropics can also be prescribed as monotherapy [22].
However, as evidenced by the publications of a number of authors [37, 111, 170], therapy based on such clinical differentiation does not always give positive results: some asthenic conditions generally show resistance to both tranquilizers and psychostimulants.
As shown by the work of A. B. Smulevich et al. [161, see also Chapter VIII], the traditional typology does not exhaust the psychopathological essence of asthenia. A clinically more significant symptom differentiating asthenic disorders is the predominance in the psychopathological structure of the syndrome of polar manifestations - hyperesthesia or hypoesthesia with alienation of one’s own activity and bodily feelings. This division allows us to significantly improve the method of psychopharmacotherapy.
In the work of L.V. Sokolovskaya [170], carried out in the clinical department of low-progressing forms of endogenous diseases and borderline mental disorders of the Scientific Research Institute of Clinical Psychiatry of the All-Russian Scientific Center for Healthcare of the USSR Academy of Medical Sciences (headed by Prof. A.B. Smulevich), in which the results of therapy of 93 patients with asthenic conditions, it is emphasized that for the phenomena of hypersthenia and hyposthenia, considered as hyperesthetic asthenia, the drugs of choice are tranquilizers and nootropics. At the same time, drug prescriptions are differentiated depending on the degree of generalization of psychopathological disorders and the psychopharmacological activity of psychotropic drugs (the concept of broad and narrow spectrum of action of 3 main classes of drugs - antipsychotics, antidepressants, tranquilizers used in the biological therapy of mental illnesses [154, 155]. Broad-spectrum drugs actions are the most universal. Possessing high psychotropic activity, such drugs are effective both in persistent, generalized and in relatively milder psychopathological disorders. The clinical activity of drugs with a narrow spectrum of action is limited to the effect on transient, relatively isolated painful manifestations.
Accordingly, for hyperesthetic asthenic syndromes with symptoms of “simple” asthenia (feeling of fatigue, increased sensitivity to external stimuli and pathological bodily sensations), narrow-spectrum tranquilizers are preferred - nozepam, mezapam, meprobamate, grandaxin, trioxazin in combination with nootropics and stimulants. In conditions with dissociation between the shallow level of asthenic disorders proper and persistent anxiety fears of hypochondriacal content, generalized conversion manifestations and other pathological bodily sensations (conversion asthenia, asthenic hypochondria), broad-spectrum tranquilizers are indicated: Relanium, phenazepam, Elenium, administered parenterally if necessary. Nootropics and stimulants, in some cases increasing irritability and vegetative motor hysterical manifestations, are prescribed in smaller doses than for “simple” asthenia and in shorter courses (1-2 weeks).
If significant improvement up to a complete reduction of painful manifestations can be achieved in the majority of patients with hyperesthetic asthenia (according to L.V. Sokolovskaya, in 69.4%) [170], then cases of hypoesthetic asthenia with alienation of one’s own activity and bodily feelings are resistant to traditional therapy using tranquilizers, nootropics and psychostimulants. At the same time, a comparison of the effectiveness of psychotropic drugs of various classes shows that in some cases such therapeutic resistance is relative. In 1/2 of the patients it is possible to achieve improvement with the help of neuroleptics (stelazine, trisedil, haloperidol, leponex), and in such cases intensive therapy is indicated - intravenous drip infusions of neuroleptics in combination with nootropics.
Assistance for other types of SFD (algopathic, conversion, somatization disorders) involves, in accordance with the general principles of treatment of the patient population under consideration, developed in the clinic of low-progressive forms of endogenous diseases and borderline mental disorders, Research Institute of Clinical Psychiatry of the All-Russian Research Center of Clinical Psychiatry of the USSR Academy of Medical Sciences, the use of psychotropic drugs of various classes (tranquilizers, antidepressants, antipsychotics, nootropics, psychostimulants), as well as somatotropic drugs (b-blockers, calcium channel blockers, antihypertensive drugs) Tranquilizers are most often used. According to A. B. Smulevich et al. [158], they are used as monotherapy (39.8% of all cases) or in combination with other psychotropic drugs: antidepressants (27.5%), antipsychotics (18.5%), nootropics (14.2%). Most often, drugs are prescribed orally in small and medium doses (Table 1). However, in case of severe dysfunction of internal organs (dyskinetic disorders of the gastrointestinal tract, cardiac arrhythmias and conduction disorders, etc.), as well as in combination. It is advisable to administer drugs parenterally (including intravenous drip) according to appropriate methods [157, 405].
Table 1. Doses of drugs (in mg/day) used in the treatment of patients with FMS
| A drug | Average dose | Highest dose | ||
| orally | parenterally | orally | parenterally | |
| TRANQUILIZERS | ||||
| Elenium | 30 | 40 | ||
| Sibazon (Relanium) | 30 | 60 | 30 | 80 |
| Lexotan | 6 | 17 | ||
| Phenazepam | 2 | 3 | 3 | 4 |
| Nozepam (tazepam) | 30 | 40 | ||
| Rudotel | 30 | 40 | ||
| Grandaxin | 150 | 200 | ||
| ANTIDEPRESSANTS | ||||
| Amitriptyline | 100 | 60 | 200 | 60 |
| Melipramine | 100 | 75 | 200 | 100 |
| Anafranil | 100 | 75 | 200 | 100 |
| Ludiomil | 100 | 75 | 200 | 100 |
| Pyrazidol | 150 | 250 | ||
| Incazan | 100 | 200 | ||
| NOOTROPICS | ||||
| Nootropil (piracetam) | 1600 | 2000 | 2400 | 4000 |
| Pyriditol (encephabol) | 400 | 800 | ||
| NEUROLEPTICS | ||||
| Triphthazine (stelazine) | 10 | 5 | 20 | 15 |
| Haloperidol | 6 | 5 | 12 | 10 |
| Trisedyl | 1,5 | 2,5 | 3 | 5 |
| Leponex | 50 | 200 | ||
| Chlorprothixene | 50 | 150 | ||
| Etaperazine | 16 | 50 | ||
| Neuleptil | 10 | 30 | ||
| Teralen | 15 | 50 | 30 | 150 |
| Sonapax | 30 | 100 | ||
| Eglonil | 300 | 200 | 400 | 400 |
| NORMOTIMICS | ||||
| Finlepsin | 200 | 600 | ||
| PSYCHOSTIMULANTS | ||||
| Sidnocarb | 10 | 30 | ||
Reversal of symptoms is observed within a month from the start of therapy. However, the tendency toward repeated exacerbation and chronicity inherent in SFR makes it advisable in some cases to continue treatment with maintenance doses. Maintenance therapy is usually provided in an outpatient setting in accordance with generally accepted principles [140, 154].
As shown by the experience of the staff of the clinical department of low-progressive forms of endogenous diseases and borderline mental disorders of the Scientific Research Institute of Clinical Psychiatry of the All-Russian Scientific Center for Healthcare of the USSR Academy of Medical Sciences, which was carried out not only in a sanatorium-type psychiatric hospital, but also in the faculty therapy clinic (head of the department - Prof. V. I. Makolkin) Moscow Medical Academy (rector - Prof. M. A. Paltsev), Moscow territorial clinic No. 171 of the Leninsky RZO (chief doctor G. A. Kazmina), city multidisciplinary hospital No. 15 (chief doctor O. N. Filatov), large Some patients with SFR (about 2/3) can be treated in a general somatic network (outpatient in a territorial clinic or inpatient in a multidisciplinary hospital) and only 1/3 need specialized psychiatric care (office or neurosis clinic, neuropsychiatric dispensary) [66].
When treated in a general somatic network, psychotropic drugs can be prescribed by a general practitioner with the advisory participation of a psychiatrist.
A special place in the treatment of the conditions under consideration belongs to tranquilizers. Drugs of this class and other psychotropic drugs (antidepressants, antipsychotics, nootropics and stimulants), according to A. B. Smulevich et al. [158], based on a personal examination of 898 patients and analysis of medical documentation (2719 medical histories, outpatient records, 24530 prescriptions), were prescribed in 80.0, 7.3, 6.8 and 5.9% of cases, respectively.
The effectiveness of monotherapy with tranquilizers is evidenced by the conclusions of a joint study carried out in the clinic of low-progressing forms of endogenous diseases and borderline mental disorders of the Scientific Research Institute of Clinical Psychiatry of the All-Russian Scientific Center for Healthcare of the USSR Academy of Medical Sciences and at the Department of Clinical Pharmacology (headed by Prof. V. G. Kukes) of the Moscow Medical Academy, based on the results therapy of 200 patients with functional cardiac disorders [159]. The authors emphasize that in more than 1/3 of cases, the use of only drugs of this class (Elenium, Nozepam, Mezapam, Sibazon, Lexotan, Grandaxin) is accompanied by a complete reduction of painful manifestations.
Clinical manifestations of SFD, the psychopharmacotherapy of which is carried out in a specialized office of a territorial clinic, a psychoneurological dispensary or a psychiatric hospital (sanatorium-type department), are limited to persistent conversion, somatization and algopathic disorders, often combined with anxious and affective manifestations. Such conditions in traditional domestic taxonomy are considered within the framework of protracted hypochondriacal reactions and development.
Below we will dwell on the principles of treatment for SFD, which require specialized treatment, using the model of the two most common, according to most researchers [209, 281, 411], forms of SFR - somatization and algopathic disorders.
For this purpose, from all the data at our disposal regarding the psychopharmacotherapy of SFR, carried out in the clinical department of low-progressive forms of endogenous diseases and borderline mental disorders of the Scientific Research Institute of Clinical Psychiatry of the All-Russian Scientific Center for Clinical Psychiatry of the USSR Academy of Medical Sciences, Moscow Psychoneurological Dispensary No. 18 (chief doctor A. V. Ukrainskikh), in the neurosis room of the Moscow Polyclinic No. 171, 295 observations were selected (133 men, 162 women, average age 36.5 ± 8.4 years) with clinical manifestations corresponding to somatization and algopathic disorders. In accordance with the differentiation of SFR proposed by M. O. Lebedeva (see Chapter VI), 255 observations (116 men, 149 women, average age 35.3 ± 7.2 years) and isomorphic ( with uniform manifestations) type - 40 patients (17 men, 23 women, average age 38.2±6.3 years).
Retrospective analysis of treatment results was ensured by the use of medical documentation data (medical histories, outpatient records), which made it possible not only to carry out a typological differentiation of FDS, but also to establish the clinical characteristics of the reverse development of FDS, as well as the use during therapy of formalized cards containing both standardized scales (questionnaires ), filled out by patients, as well as information on medication prescriptions grouped by courses (monotherapy with tranquilizers, monotherapy with neuroleptics, neuroleptic and tranquilizer, tranquilizer and antidepressant, neuroleptic and antidepressant, tranquilizer and nootropic, neuroleptic and nootropic, monotherapy with antidepressants, monotherapy with nootropics, monotherapy with finlepsin , antidepressant and nootropic, tranquilizer and finlepsin, antipsychotic and finlepsin, antidepressant and finlepsin, nootropic and finlepsin) (Table 2).
Table 2. Frequency of use of various courses of treatment in patients with different types of FDS
| Treatment | Courses | |
| Abs. | % | |
| Monotherapy with tranquilizers | 70 | 12,3 |
| Monotherapy with antipsychotics | 25 | 4,4 |
| Tranquilizer and antidepressant | 179 | 31,5 |
| Neuroleptic and tranquilizer | 83 | 14,7 |
| Tranquilizer and nootropic | 34 | 6,0 |
| Neuroleptic and nootropic | 29 | 5,1 |
| Neuroleptic and antidepressant | 104 | 18,3 |
| Monotherapy with antidepressants | 2 | 0,4 |
| Monotherapy with nootropics | 3 | 0,5 |
| Finlepsin monotherapy | 7 | 1,2 |
| Antidepressant and nootropic | 4 | 0,7 |
| Tranquilizer and finlepsin | 8 | 1,4 |
| Neuroleptic and finlepsin | 7 | 1,2 |
| Antidepressant and finlepsin | 6 | 1,1 |
| Nootropic and finlepsin | 7 | 1,2 |
| TOTAL: | 586 | 100,0 |
The distribution of the listed courses of therapy by frequency of use, regardless of the type of SFR, shows a preference for the first 7, while the rest accounted for a total of 7.6% of the total number of courses with a relatively even distribution. Courses of therapy that were used less frequently than others, and therefore are not of fundamental importance from the point of view of statistical processing of the material, are combined and designated as “other psychotropic drugs and their combinations.”
Data on the effectiveness of various courses of drug therapy in patients with polymorphic and isomorphic types of FMS are presented in Table. 3.
Table 3. Comparison of the effectiveness of various courses of treatment in patients with polymorphic and isomorphic types of FMS
| A course of treatment | SFR | R | ||||
| isomorphic | polymorphic | |||||
| Total courses | effective | Total courses | effective | |||
| Monotherapy with tranquilizers | 30 | 3** | 40 | 27 | 8,82 | <0,01 |
| Monotherapy with antipsychotics | 14 | 9 | 21 | 0** | 7,66 | <0,01 |
| Tranquilizer and antidepressant | 8 | 0** | 171 | 129 | 4,28 | <0,05 |
| Neuroleptic and tranquilizer | 30 | 12 | 53 | 10 | 2,45 | >0,05 |
| Tranquilizer and nootropic | 16 | 2** | 18 | 14 | 4,23 | <0,05 |
| Neuroleptic and nootropic | 11 | 8 | 18 | 0** | 7,34 | <0,01 |
| Neuroleptic and antidepressant | 25 | 13 | 79 | 2** | 209,07 | <0,01 |
| Other psychotropic drugs and their combinations | 15 | 3** | 29 | 2** | 0,42 | >0,05 |
| For all courses: | 149 | 48* | 429 | 198 | 3,56 | >0,05 |
* - the number of effective courses may exceed the number of observations, since the majority of the examined patients received therapy not only at initial treatment, but also for deterioration of their condition during follow-up observation ** - with the number of observations not exceeding 5, chi-square was used when calculating the value Yates' amendment.
Before moving on to the discussion contained in the table. 3 data, it should be indicated that the effect of each individual course of treatment was assessed in accordance with. the sum of scores on the somatization scale of the structured Hopkins questionnaire in patients with the polymorphic type of FMS [285] or on the McGill scale in patients with the isomorphic type of FMS [83]. The response to treatment was considered negative if the initial sum of scores on the scales used did not change, and positive if the sum of scores decreased by 50% or more.
Thus, for each type of SFR, the total number of treatment courses and the number of effective courses were recorded. The corresponding indicators presented in table. 3, are expressed in absolute numbers, which makes it possible to use the chi-square test when comparing the effectiveness of different courses of treatment in patients with polymorphic and isomorphic types of SFR.
Thus, it can be seen that there are no statistically significant differences in the overall effectiveness of all completed courses of therapy, as well as the effectiveness of such combinations as an antipsychotic and a tranquilizer, “other psychotropic drugs and their combinations” in the treatment of patients with polymorphic and isomorphic types of FDS.
However, upon further analysis of the treatment results, it is noteworthy that in patients with the polymorphic type of FMS, the effectiveness of treatment courses that included tranquilizers, both as monotherapy and in combination with antidepressants and nootropics, is higher than the effectiveness of the same medications in patients with the isomorphic type of FMS (the differences are statistically significant). In these patients, monotherapy with neuroleptics and a combination of drugs of this class with antidepressants or nootropics can be considered the most effective, on statistically significant grounds, but the same therapy in patients with the polymorphic type of SFR practically does not lead to an improvement in the condition.
It can be assumed that the positive results of therapy for patients with the polymorphic type of FMS are determined by the prescription of tranquilizers, while in patients with the isomorphic type of FMS - antipsychotics.
To test this assumption, it is advisable to compare the overall effectiveness of therapy for all courses in patients with each of the studied types of SFR using tranquilizers both as monotherapy and in combination with antidepressants and nootropics, and antipsychotics in combination with antidepressants and nootropics (Table 3 ).
The effectiveness of the first set is compared in patients with the polymorphic type of FDS with the overall effectiveness of all courses of treatment in patients with the type of FMS under consideration; in the same way, the effectiveness of the second set of courses in patients with the isomorphic type of SFR is compared with the overall effectiveness of all courses in the same patients in combination with antidepressants and nootropics (see Table 3). The effectiveness of the first set is compared in patients with the polymorphic type of SFR with the overall effectiveness of all courses in these same patients.
This analysis allows us to establish the following differences. The first 3 courses of treatment (monotherapy with tranquilizers, a tranquilizer and an antidepressant, a tranquilizer and a nootropic) in total are significantly more effective in patients with the polymorphic type of SFR (x2=18.19; df=1; p<0.05); in the treatment of isomorphic type SRF, a combination of courses such as monotherapy with neuroleptics, a neuroleptic and an antidepressant, an antipsychotic and a nootropic is significantly more effective (x2=4.85; df=1; p,0.05).
In other words, tranquilizers can be recommended first of all as the drugs of choice when treating patients with the polymorphic type of FPS, and antipsychotics in patients with the isomorphic type of FPS.
If the total positive effect of the preferred courses of treatment (monotherapy with tranquilizers, a tranquilizer and antidepressant, a tranquilizer and a nootropic) in patients with the polymorphic type of FDS reaches 80.3%, then the most effective courses of treatment for a relatively small group of patients with the isomorphic type of FDS (monotherapy with neuroleptics, an antipsychotic and antidepressant, antipsychotic and nootropic) lead to improvement in only 60% of observations (T = 3.05; p <0.01). Consequently, isomorphic type SRFs are more resistant to therapy.
In conclusion, it is necessary to provide some clinical characteristics of the reverse development of FDS. studied types in cases where therapy was accompanied by a positive effect.
The reduction of painful manifestations in SFR of the polymorphic and isomorphic types reveals features that are apparently associated with psychopathological differences between these types of somatization. In case of diverse polymorphic type SFRs, variable in localization and severity, there is no preferable medicinal effect on one or another sign (or several signs) belonging to both the somatopsychic (functional disorders of internal organs, pathological bodily sensations) and autopsychic (anxiety-phobic disorders) spheres. The weakening of pathological bodily sensations, as well as symptoms of the autopsychic sphere, when reduced in any sequence, is accompanied by an improvement in general well-being and the restoration of full social functioning.
Other dependencies were noted in the process of reducing psychopathological disorders in patients with the isomorphic type of SFR. With this type, a clinically registered improvement in condition is observed only if the severity of pathological bodily sensations decreases.
SUMMARY
Recommendations for the treatment of SPS, developed in the clinic of low-progressive forms of endogenous diseases and borderline mental disorders of the Scientific Research Institute of Clinical Psychiatry of the All-Russian Scientific Center for Healthcare of the USSR Academy of Medical Sciences, are presented. About 2/3 of patients with SFR can be treated in a general somatic network (outpatient in a territorial clinic or in a multidisciplinary hospital). In this case, psychotropic drugs are prescribed by a general practitioner with the advisory participation of a psychiatrist. 1/3 of patients with SFR need specialized psychiatric care (neurosis room, psychoneurological dispensary, neurosis clinic, sanatorium department of a neuropsychiatric hospital). When treating SFR, psychotropic drugs of various classes are used (tranquilizers, antidepressants, neuroleptics, nootropics, psychostimulants), as well as somatotropic drugs ((3-adrenergic blockers, calcium channel blockers, antihypertensive drugs). In case of severe dysfunction of internal organs (dyskinetic disorders of the gastrointestinal tract) - intestinal tract, vegetative crises, cardiac arrhythmias, etc.), as well as in combinations of SFR with anxious and/or affective disorders, it is advisable to administer medications parenterally (including intravenous drips). In the treatment of a variety of conversion, somatization, algopathic disorders, and Also, the phenomena of hyperesthetic asthenia are most widely used by tranquilizers, both in the form of monotherapy and in combination with other psychotropic drugs.In the treatment of a relatively small group of SFRs, the clinical picture of which is limited to persistent algias of the idiopathic type or other isomorphic disorders, as well as hypoesthetic (autochthonous) asthenia With the alienation of one’s own activity, neuroleptics (haloperidol, stelazine, leponex) are most effective, if necessary in combination with tranquilizers and antidepressants.
SUMMARY
Given here are the recommendations for somatoform disorders (SFD) therapy. It turned out that the majority of SFD patients (about 2/3) can undergo regular treatment in the general somatic network (both outpatient and territorial policlinic in-patient hospitals). In such cases psycho tropic drugs are advised by the general practitioner together with a consulting psychiatrist. /z of SFD patients need a special psychiatric aid (psychiatric out - and - in patient departments). The SFD therapy uses different classes of psychotropic drugs - tranquillizes, anti-depressants, neuroleptics, noot-tropic drugs, psycho stimulants, as well as somatotropics - adreno-blockers, calcium channel bloekers, hypotensive drugs. Drugs are advised parentally (also in the form of intravenous drops) at marked vegetative dysfunctions (stomach-intestinal dyskenesias, vegetative crises, cardiac arrythmia and others), as well as at SFD combination with anxious and/or affective disorders. The tranquilzes used both at monotherapy and in combination with psychotropic drugs are more widely used in the treatment of diversiform conver-sional, somatization and algic disorders. In the treatment of relatively small SFD group, characterized by isolated stable idiopathic algias, or other isomorphous SFD as well as hypersensitive (autochthonous) asthenia with alienation of self-activity, the neuroleptics (haloperidol, stellazin, leponex), combined if necessary with tranquillizers and antidepressants are the most effective.
Somatization and chronic somatoform pain disorder
Somatized dysfunction, in addition to organ manifestations, causes a decrease in the functioning of analyzers: vision, hearing, touch, smell. Coordination of movements is impaired: patients become clumsy and have an unsteady gait. Movement disorders manifest themselves in the form of paresis and paralysis.
They describe failures in the functioning of internal organs colorfully and with charm. For example, my head hurts, as if a hoop was put on it and was gradually being squeezed. Or your stomach is swollen like a balloon.
Unlike a hypochondriac, who expresses anxiety about his health, such a patient responds more rudely and persistently. He is convinced that he is sick. And if the doctor tries to hint at the psychogenic nature of the disorder, he screams and is indignant, rejecting what was said, and demands additional examination. This patient is constantly dissatisfied and complains.
The course of the disease is chronic, with wide variability of symptoms that persist for 2 years or more.
Often, a person, due to his anxiety and aggressiveness, experiences social maladjustment and family conflicts.
A pain disorder is distinguished by the presence of severe, debilitating pain that occurs for no reason. Usually it has a clear localization - the stomach, the heart. The pain characteristics do not change, there are no other symptoms.
During somatoform dysfunction, an undifferentiated disorder is also distinguished. With it, a person suffers all the typical symptoms of the disease, but it is not possible to classify them into any known group.
How is the treatment carried out?
The basis of the rehabilitation course includes both taking medications and periodic work with a psychiatrist.
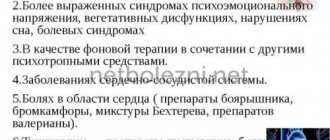
Patients are prescribed the following groups of drugs:
— Tranquilizers with sedative effects (for example, phenazepam); — Antidepressants that improve emotional state and neutralize the state of apathy; - Neuroleptics (for example, Sonapax), which block the feeling of panic and anxiety; - Beta blockers (for example, propranolol), which neutralize trembling, sweating and other manifestations of autonomic manifestations.
Somatoform dysfunction of the autonomic nervous system
The syndrome develops when there is a malfunction of the autonomic nervous system, which controls the functioning of internal organs, blood vessels, and is responsible for the course of physiological processes and the mobilization of the body as a whole.
The ANS consists of 2 sections: parasympathetic and sympathetic.
The sympathetic nervous system increases the heart rate, constricts blood vessels and increases blood pressure. Increases sweating and slows down intestinal motility. It relaxes the bladder, dilates the bronchi and pupil. Sympathy speeds up metabolism and activates the body as a whole.
The parasympathetic system has the opposite effect. But, despite the opposition of departments, normal well-being of a person is ensured by their coordinated work. Any malfunctions in the functioning of both systems cause various pathological sensations and syndromes, in particular, somatoform dysfunction.
There are 3 types of disorders:
- with a predominance of sympathy;
- with a predominance of parasympathetics;
- mixed.
According to the flow, stable and paroxysmal, with vascular and other types of crisis are distinguished.
Pathology can be primary, that is, it develops on its own, or secondary, after previous illnesses. Its symptoms manifest themselves under the influence of a psychotraumatic factor.
Such patients are characterized, first of all, by the appearance of vegetative signs: severe sweating, tremors of the limbs, paleness and redness of the skin.
Another group of signs expresses the dysfunction of internal organs under the control of the ANS:
- cough, shortness of breath, laryngeal spasm;
- tachycardia, arrhythmia, blood pressure changes. Heart pain does not have a clear localization and can be of various types. It happens that they are accompanied by a feeling of anxiety or fear. They are worse at rest, but go away during physical activity. Lasts from a few minutes to several days. Heart symptoms are so believable that they sometimes confuse even specialists;
- abdominal pain, bloating, difficulty swallowing; “bear disease” - diarrhea under the influence of stress;
- difficulty urinating, urinary incontinence;
- headaches, fatigue, poor sleep.
The complaints are numerous, but lack specifics. They signal a disruption in the functioning of several organs at once.
Patients are concerned about their condition, but still not to the same extent as hypochondriacs. They strive to find a way out of the situation and receive adequate treatment.
What can cause the disorder
The process of formation of somatoform disorders has not yet been well studied. The most relevant theory today is the neuropsychological concept. Its creators suggest that people suffering from various types of somatoform disorders have a low pain threshold. They simply cannot tolerate physical discomfort, and what others would consider to be some kind of tension is perceived by sick people as severe pain. The trigger for pathology is often a stressful situation that has great personal significance. Usually these are constant stress at work or at home, as well as other troubles that seem insignificant from the outside.
Factors that can lead to the development of somatoform disorders are divided into three large groups:
- hereditary and constitutional factors. This group includes features of the functioning of the central nervous system and character. Born pessimists, hypochondriacs, as well as overly timid and shy people are at risk;
- psycho-emotional factors, in turn, are divided according to the strength of their impact. Massive factors are often catastrophic in nature, appear suddenly and greatly shock. Acute situational factors are associated with some damage to self-affirmation, this could be the loss of a job or social status. Prolonged situational factors may be due to various psychological reasons. For example, a person may have personal aspirations that do not correspond with his capabilities to achieve the desired goal;
- organic factors can also lead to the development of somatoform disorders. Most often, mental disorders are associated with a malfunction of the central nervous system caused by injuries, infectious diseases, toxic effects, etc.
External factors can have different scales of impact. Restrictions on the expression of emotions may be imposed by cultural, ethnic or religious traditions (cultural-ethnic factors). But at the same time, there are families in which a child can receive the desired love and care only at the time of illness, and the rest of the time he must suppress external manifestations of emotions (microsocial factors)
SDVNS in children
Often, somatoform autonomic disorder appears in children at puberty, that is, during the period of maturation. This is due to a hormonal surge and intensive growth of the body.
The following factors can provoke the process:
- heredity;
- stress;
- mental, physical stress;
- infections;
- bad habits;
- surgical interventions;
- large body weight;
- sedentary lifestyle;
- staying at the computer for a long time.
The appearance of teenagers is typical. If sympathy predominates, then the skin of such children is moist and oily, with acne. She alternately turns red and pale. A bluish tint appears. Cold, with a marbled pattern called a vascular necklace. When pressed with a finger, the skin turns pale and red dermographism is observed.
When parasympathetics dominate, the skin is dry, with pink or white dermographism. These children have an increased appetite, but they do not gain weight.
The disorder is accompanied by a sudden rise in temperature under the influence of stress. A typical occurrence is fainting.
All characteristic changes in internal organs are present.
The psycho-emotional sphere is also undergoing changes. Such a child becomes distracted and nervous. He quickly gets tired, drowsiness and apathy appear, and his memory deteriorates.
In most cases, the course of the disease is stable. But periodically panic attacks and crises occur:
- sympatho-adrenal - accompanied by tachycardia, elevated blood pressure, headaches, thirst, chills and hyperthermia. Anxiety and feelings of fear develop;
- vagoinsular – migraine-like attacks, nausea, vomiting, pain in the abdominal area. Hyperhidrosis, decreased blood pressure and fainting, slow heart rate, increased urine output, breathing disorders;
- mixed.
The attack can last up to several hours.
Diagnostics
The main task at the stage of diagnosing the disorder is to exclude somatic causes of pain and other patient complaints. The diagnosis of “somatoform disorder” is made if the patient’s multiple and inaccurate complaints do not find laboratory and instrumental confirmation. In this case, the patient’s medical history must include previous examinations, the results of which were not satisfactory to him.
Additional confirmation of the diagnosis may include peculiar reactions to diagnostic procedures and therapy:
- all manipulations carried out to diagnose the disease cause paradoxical relief in the patient;
- somatic symptoms, which act as the main manifestation, can be changed by the patient. Typically, this trend is observed from exacerbation to exacerbation, but symptoms can change within the same episode;
- therapeutic treatment does not give a sustainable result;
- The patient clearly shows a tendency to idiosyncratic reactions.
The difficulty in diagnosing somatoform disorders lies in the inability to differentiate them from many other mental illnesses in which patients also complain of physical illness. Such disorders include depression, hypochondriacal delirium, etc. The doctor must also take into account the fact that the patient may have the initial stage of a true somatic disease.
Revealing
It is about such complaints that the patient goes to the doctor, most often a therapist or neurologist. Experienced doctors usually identify somatoform disorder during consultation. Sometimes doctors need additional examinations that show the norm, which confirms the diagnosis.
Such a patient is referred to a psychotherapist or psychiatrist. Very often the patient denies the neuropsychic origin of his complaints and even resists attempts to discuss this cause. Therefore, the doctor (and the patient’s loved ones) should be patient in persuasion.
In practice, unfortunately, such patients will change several doctors, undergo many tests (all studies will show the norm) before they get to a specialist who can help them!