A person gets acquainted with the world around him through direct contact with it, through sensations and perceptions.
These two components of the general process of sensory cognition play a huge role and are inextricably linked with each other.
Sensations help to gain knowledge about color, sound, temperature, taste, and perception puts it all into an overall holistic picture.
Phenomenology of Perceptual Disorders
Perception is an active process of analyzing and synthesizing sensations by comparing them with previous experience.
Perception, unlike sensations, is holistic in nature and is a visual-figurative reflection of objects and phenomena acting on the senses at the moment.
In the world literature on psychopathology, there are descriptions of the following perception disorders:
1) hypersthesia - increased perception of strength;
2) hyposthesia - weakening of perception of strength;
3) agnosia - lack of recognition;
4) total anesthesia - loss of sensitivity during hysteria;
5) depersonalization - a disorder in the perception of one’s own personality;
6) poverty of participation - loss of complex feelings;
7) derealization - distorted perception of the surrounding world. This also includes the symptoms of “already seen” (de ua vu), “never seen” (ua mais vu);
 deceptions of perception (illusions and hallucinations).
deceptions of perception (illusions and hallucinations).
Domestic research in general psychology is characterized by an approach to perception as an activity. Accordingly, our pathopsychologists consider disturbances of perception as a disorder of certain characteristics of activity.
These violations manifest themselves:
1) difficulty in recognition (agnosia);
2) in distortions of the perceived material (pseudognosia);
3) in deceptions of the senses (hallucinations);
4) in false recognitions (pseudohallucinations);
5) in restructuring the motivational side of perceptual activity (perceptual defenses, altered meanings). Let's look at them in more detail.
Examples of illusions in psychology
Widely known examples of perceptual distortions are fractal pictures. In fact, the images are static, but if you look closely at their central part, it seems as if it is moving.
Cognitive illusions manifest themselves through certain stereotypes, for example:
- fat people are good-natured, thin people are evil;
- the dog is angry, the cat is affectionate;
- dolphins save people;
- in life you need to achieve success (plant a tree, raise a son, ...);
- The necessary knowledge can only be obtained by entering an educational institution.
You can encounter illusion in everyday life. For example, if you look closely at the railway track, it seems that at a distance it is narrower than up close.
In psychology, some illusions are used for diagnosis. Thus, Rorschach blots are an example of a deliberately induced illusion used to reveal the intellectual abilities and other characteristics of the subject.
Irina Sherbul
Agnosia
Agnosia is a disorder of recognition. And in more detail, it is a disorder of recognition of objects, phenomena and parts of one’s own body while maintaining consciousness of the external world and self-awareness, as well as in the absence of disturbances in the peripheral and conductive parts of the analyzers.
There are three types of agnosia: visual, auditory and tactile. Visual agnosia, in turn, is divided into:
1) object agnosia (patients do not recognize objects and their images). This group also includes Wolpert’s “simultaneous agnosia” (patients recognize individual objects and their images, but do not recognize the situation as a whole);
2) agnosia for colors and fonts;
3) optical-spatial agnosia (the ability to convey the spatial characteristics of an object is lost: further, closer, more, less, above, below, etc.).
Auditory agnosia manifests itself in a decrease in the ability to differentiate sounds and understand speech. In this case, auditory hallucinations may occur. Defects in auditory memory are possible (patients cannot remember two or more sound standards). Arrhythmia is possible (they cannot correctly assess rhythmic structures, the number of sounds and the order of alternations). Sometimes there is a violation of the intonation side of speech (patients do not distinguish between intonations and they themselves have inexpressive speech).
Tactile agnosia - when tactile sensitivity is preserved, there is a failure to recognize familiar objects when they are perceived by touch (examination with eyes closed).
Agnosia in mentally ill patients manifests itself in the fact that they highlight first one or another sign of a perceived object, but do not recognize the object itself.
Such disorders more often occur with organic lesions of the cortical areas of the brain of various origins (encephalitis, tumor, vascular process, etc.).
Let us give examples of observations and experimental studies carried out by different authors (mostly graduate students of B.V. Zeigarnik).
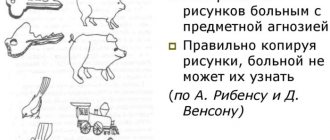
Example 1. One patient describes the image of a nail as something round, saying: “there’s a cap on top, a stick on the bottom, I don’t know what it is.”
Example 2. Another patient describes the key as “ring and rod”, he can even copy it exactly, but this does not make it easier to recognize.
Example 3. When tachistoscopically presented with a garden watering can, the patient says: “A barrel-shaped body, something round, in the middle it comes off like a stick on one side.” Another patient, when tachistoscopically presented with a comb, says: “Some kind of horizontal line, small, thin sticks extend from it downward.”
Example 4. The patient calls the drawn mushroom a “haystack,” and the matches “crystals.” The patient does not grasp the plot of the picture immediately, but only after long fixations on individual details. The process of perception is in the nature of guessing: “What could this be - a comb? What is she sitting on - an armchair, a stool? What could it be - a stove, a trough? Looking at the painting “Suicide Woman,” the patient says: “What kind of woman is this, thinking about something? What is she sitting on? On the bed? What are these shadows?
With such a pronounced impairment in drawing recognition, the patient perfectly recognized geometric shapes and completed unfinished drawings in accordance with structural laws. Moreover, without recognizing the object in the drawing, the patient perfectly described its shape.
Summing up a series of similar experiments, B.V. Zeigarnik came to the conclusion that there is a certain gradation of disorders in agnosia. The patients recognized objects well, models less well, and drawings of objects even worse. They recognized especially poorly those images that were schematically drawn in the form of outlines.
A hypothesis arose that the reason for the difficulty of recognition is caused by the generality, the formalization that is inherent in the drawing.
To test the hypothesis, a series of experiments was carried out: patients were presented with images of the same objects in different executions:
a) in the form of a dotted outline;
b) in the form of a black silhouette;
c) in the form of a clear photographic image.
The data from the experimental study confirmed the assumption: the patients did not recognize dotted images at all, they recognized silhouette images somewhat better, but still very poorly, and they recognized photographic, i.e., concrete images, better.
Hence the conclusion was drawn: perception during agnosia, in its specifically human characteristics, is a process that has the function of generalization and convention; Therefore, here it is legitimate to talk about a violation of the generalizing function of perception.
Knowledge of the psychological mechanism of agnosia made it possible to select methods by which this defect could be compensated. Thus, if the experimenter asked to indicate a certain object (“indicate where the hat is and where the scissors are”), then the patients recognized it and completed the task correctly. That is, the inclusion of the presented object in a certain (not requiring a generalization operation) circle of meaning helped recognition. Naming the approximate circle of objects to which a given object belongs (show a headdress, a tool) helped less.
Major Perceptual Disorders
Psychiatry as a field of clinical medicine operates in terms of methodology, diagnosis, treatment and prevention. To make a diagnosis, it is necessary to clearly know the manifestations of the disease; clinical tests, medical history, laboratory and instrumental studies help with this. The categorical nature of judgments allows one to correctly interpret the data obtained in order to make an adequate diagnosis. In psychiatry, there are two main categories of perceptual disorder to refer to certain mental health problems:
- illusions;
- hallucinations.
Both concepts evoke quite negative feelings in most people, but the patient himself has no control over them, although in many cases such disorders occur due to conditions into which a person has driven himself, for example, drug or alcohol poisoning. Some types of perception disorders can occur in completely healthy people in terms of psychiatry.
Pseudoagnosia in dementia (False misrecognitions in dementia)
A study of visual perception in patients whose clinical picture and experimental psychological studies revealed dementia of the organic type revealed the above-mentioned features: the patients did not recognize silhouette and dotted patterns. But another feature was added to this: their perception was diffuse, undifferentiated. The object of recognition was determined by the part of the drawing on which the patient fixed his attention. Let us give the most striking examples according to B.V. Zeigarnik.
Example 1. A patient calls a mushroom a tomato if he looks at the head of the mushroom, or sees a cucumber in the mushroom if he fixes his attention on its stem. Therefore, when presenting a drawing to a patient, it is often indifferent whether they show him part or the whole of it.
In some patients, agnosia extended to both the structure and shape of the image.
Example 2. When shown a triangle, the patient says: “Something like a wedge, but I can’t call it, I see a wedge in three places, a wedge-three-wedge.” When exposing the quadrilateral, the patient says: “It’s hard for me to say (circles with a finger) - straight, straight, straight and straight.” When exposing an unfinished circle, he sees first of all the flaw: “There is some kind of failure here,” while at the same time he perceives the symmetry of the form. For example, when showing a cross, not being able to name the figures, the patient declares: “Look wherever you want, it lies correctly.”
Example 3. When examining a picture of a peasant standing with a thoughtful look by a cart whose wheel has bounced off, the patient says: “Here is the wheel, and this is a man standing.” Pointing to the horse, he says: “And this is some kind of bird.” Experimenter: “It’s a horse.” Patient: “It doesn’t look like a horse.”
In these examples, there is a clear violation of not only the semantic, but also the structural components of the drawing. When trying to understand the plot of a picture, patients often incorrectly describe its content due to incorrect recognition of details and structural decay. This disorder resembles the phenomenon described by A. Pick as “senile agnosia” or as a disorder of “simultaneous perception”. It is expressed in the fact that the subject, while describing individual objects, is unable to grasp the general meaning of the picture.
As we see, the disturbance of perception that is found in mentally retarded patients confirms the leading role of meaningfulness and generalization in any act of perceptual activity. Thus, pathological material reveals the integrity of mental (reflective) activity. The considered disturbance of perception is, in fact, a violation of mental operations - synthesis and generalization.
Perceptions and medical practice
If any disturbances occur in the human body, a big problem may arise - perception disorders. Psychiatry, as a scientific and practical field of medicine, studies these disorders and, as far as possible, helps correct them. Psychiatrists have been studying perception disorders for centuries, helping not only the patients themselves, but also the people around them, to live with such problems. Disturbances in the functioning of one or more sense organs are not always disorders of a complex analysis of the surrounding world. A person who has lost his sight knows what objects and colors really look like and, with the help of the other senses, can imagine a real picture of the world around him. In psychiatry, disorders of the perception process are a whole complex of disorders caused not so much by problems in the functioning of receptors, but by changes in the processes of processing received information and obtaining the final result.
Deceptions of the senses
Hallucinations and their types
Hallucinations in psychiatry are false perceptions. In mental illness, this is one of the most common symptoms.
Hallucinations come in different modalities: patients see objects that are not there, hear speech, words that are not spoken by anyone, smell smells that do not really exist. Based on the type of analyzer, visual, auditory, olfactory, gustatory and other hallucinations can be distinguished.
Even the French psychiatrist E. Esquirol wrote that a hallucinant is “a person who has an internal conviction that he perceives something, while there is no object from the outside that can cause this perception.”
This definition by Esquirol formed the basis for the opinion of psychiatrists that hallucinations occur without the presence of a stimulus. However, as we will see later, this is not entirely true. Illusions should be distinguished from hallucinations.
Illusions are a distorted perception of a real object that actually exists in the external environment.
Thus, in traditional psychiatry, depending on the presence or absence of a stimulus, sensory deceptions are classified as illusions or hallucinations.
Features of hallucinatory images
There are seven features that distinguish hallucinatory images from ordinary ones:
1. The patient’s attitude towards hallucinations and their impact on the patient may be different:
- there is a neutral attitude when patients calmly react to them;
- hallucinations can be imperative in nature, when a voice orders the patient to do something, for example, “burn your things” or “throw away money”;
- “voices” can be frightening, for example, they threaten to kill. Under the influence of such voices, patients can perform certain actions (for example, the mentioned patients actually burned things and threw away money).
2. Patients often deny the presence of hallucinations, but their behavior indicates that they are hallucinating.
For example, while talking with a doctor, a patient suddenly says to the “voice”: “Don’t bother me, you see, I’m busy,” another one chases away the “mice” that are supposedly crawling along his sleeve. With olfactory hallucinations, patients may refuse to eat: “It smells like gasoline, kerosene, rot.”
3. Patients, as a rule, cannot distinguish hallucinatory images from images obtained from real objects.
4. The hallucinatory image is projected outward. A patient suffering from hallucinations can pinpoint the location of the hallucinatory image. He says that this image is “to the right”, that “the car is standing below in front of the window.”
5. The hallucinatory image, as a rule, is sensually colored: patients distinguish the timbre of the “voice”, whether it belongs to a man or a woman, they see the color, bright, dark, of small or large animals. This vivid sensuality makes the hallucinatory image similar to the image obtained from real objects.
6. The hallucinatory image arises involuntarily. The patient does not expect to cause it, cannot get rid of it, hallucinations arise in addition to his desires and volitional efforts.
7. The appearance of a hallucinatory image is accompanied by a lack of criticality. It is impossible to convince the patient that the object that caused the hallucinatory image does not exist.
In support, we can cite examples taken from medical histories: “How can you not see,” the patient objects to the doctor’s assurances that there is no one in the room - after all, there is a dog standing there, over there in the right corner, ears raised, red fur, well, “Well, here she is,” or: “How come you don’t hear, because quite clearly a man’s voice orders me, “raise your hand, raise your hand, this is the hoarse voice of a smoker.”
It is useless to convince the hallucinant - the painful symptom goes away only with an improvement in the general condition.
On the mechanism of hallucinations or on the question of the nature of sensory deceptions
The question of the mechanisms of hallucinations has been raised more than once. Initially they were associated with receptor disruption; then - with a violation of certain parts of the central nervous system; finally, with the intensification of ideas (inhibitory theory of hallucinations). Let's take a closer look at the last theory.
The basis for it was the statements of I.P. Pavlov that hallucinations arise in the hypnotic paradoxical phase. Indeed, a number of clinical facts speak in favor of such a conclusion.
It was found that hallucinatory images intensify when falling asleep and at the moment of awakening; on the other hand, taking stimulant drugs such as caffeine, phenamine, weakens hallucinations, while at the same time taking inhibitory drugs (bromine, sleeping pills, phenazepam, etc.) activates the hallucinatory process.
Based on the position that during the paradoxical phase, weak stimuli acquire greater strength, and strong ones, on the contrary, are inhibited, D. B. Popov believed that ideas under the influence of hypnoid phases are intensified and projected as real objects into external space. Hence this theory is called inhibitory, and the mechanism of hallucinations, according to D. E. Popov, is the intensification of ideas.
Dissatisfied with these hypotheses, S. Ya. Rubinshtein developed the following technique: patients were offered faintly audible sounds recorded on tape, which were objective in nature (rustle of paper, gurgling of water), the nature of others was uncertain.
The experiment showed the following: while healthy subjects distinguished sound sources, in patients these experiments caused hearing deceptions. S. Ya. Rubinstein describes how one patient heard, at the sound of rustling paper, the words: “You are rubbish, you are rubbish...”, another heard sobs, the patient, a former sailor, heard the clinking of bottles, the surf of the sea.
As a result, S. Ya. Rubinshtein came to the conclusion that one of the important pathogenetic conditions for the formation of hallucinations is difficulty in listening and recognizing sounds, and if at all, difficulty in the activity of the analyzer.
This mechanism of the occurrence of hallucinations is confirmed by observations of mentally healthy people.
The literature describes cases where hallucinatory experiences occurred:
1) in conditions of sensory deficiency (among divers, people in hyperbaric and hyperbaric chambers);
2) for the visually impaired and the hearing impaired (but not for the blind or deaf).
The experiments carried out allowed S. Ya. Rubinshtein to doubt the legitimacy of defining hallucinations as false perceptions that arise without the presence of stimuli that condition them in the external or internal environment. In her opinion, it would be more correct to understand hallucinations as reactions to falsely perceived stimuli.
Pseudohallucinations
Of particular interest to a clinical psychologist is the type of hallucinatory disorder called pseudohallucinations. They were first described in detail by the Russian psychiatrist V. X. Kandinsky and the French psychiatrist P. Clerambault.
In the book “On Pseudohallucinations,” V. X. Kandinsky distinguishes pseudohallucinations from both true hallucinations and from memory images and fantasies:
1. “These images do not have the character of objective reality; on the contrary, they are directly recognized as something subjective, anomalous, very different from ordinary images of memories and fantasies.”
2. Unlike hallucinations, pseudohallucinations are projected not in external space, but in “internal” - voices sound “inside the head”, patients hear them as if in the “inner ear”; visions are perceived by the “mental” gaze, the “spiritual eyes.” For the patient, hallucinations are reality itself; pseudohallucinations are experienced by him as a subjective phenomenon. Like hallucinations, pseudohallucinations are possible in any sensory sphere: they can be tactile, gustatory, kinesthetic. But in any case, they are not identified with real objects and their qualities.
3. Unlike memories and fantastic images, pseudohallucinations seem more distinct and vivid, and the images are simultaneously in the smallest detail, persistent and continuous. Pseudohallucinations occur spontaneously, regardless of the will of the patient; they cannot be arbitrarily changed or expelled from consciousness.
4. With pseudohallucinations, there is very often no feeling of one’s own activity, activity, as is normal when a person remembers, thinks, and fantasizes. Sometimes pseudohallucinations have the character of an imposition: they are “made” by someone; patients complain that they are “forcibly shown pictures”, “causing thoughts to sound”, “acting against their will with their tongue, saying words that they do not want to pronounce”, “someone is acting with their arms, legs, body”, etc. depersonalization, which we have already described above: one’s own mental production becomes someone else’s.
Kandinsky-Clerambault syndrome
The combination of pseudohallucinations with a symptom of alienation, “made-ness” in pathopsychology is called Kandinsky syndrome.
The main radical of Kandinsky syndrome is the feeling of “made” thoughts, feelings, perceptions, the loss of their belonging to one’s own personality, the feeling of mastery, influence from the outside.
There are three components of this syndrome:
1) ideational - “made”, violence, openness of thoughts;
2) sensory - “madeness” of sensations;
3) motor - “madeness” of movements.
The nature and psychological mechanisms of this syndrome remain largely a mystery.
Why is the perception of reality disrupted?
When faced with psychiatric problems, the question arises: what are the causes of perception disorders? There can be a whole range of them: from alcohol and drug poisoning to a pathological state of the human psyche. Mental illnesses are quite difficult to diagnose, often due to the fact that a person cannot accurately describe his feelings, the events that happened or are happening to him, and the initial stages of the disease are not always noticeable to others. Perception disorders can develop as a consequence of any diseases of internal organs or systems, as well as due to disruption of the processes of processing received information, analyzing it and obtaining a specific result. Psychiatric practice at the moment cannot absolutely accurately determine the causes of the development of perception disorders, except for intoxication, when the mechanism of pathology is precisely determined by the toxic substance. Disturbances in the perception of reality can and should cause caution among people around them, since often the patients themselves are in no hurry to turn to specialists, not considering these disturbances as something pathological. A timely identified problem with the perception of surrounding reality can help the patient avoid serious problems. Distorted reality is a huge problem both for the patient and for the people around him, both mentally and physically.
Violation of the motivational component of perception
It was shown above that a decrease in generalization leads to agnosia, and changes in the functional state of the activity of analyzers lead to deceptions of the senses. Now let’s ask ourselves the question: how does a change in the motivational component of perception affect perceptual activity?
The answer to this question was obtained by B.V. Zeigarnik and the staff of her laboratory in a study of the perception of patients with the so-called frontal syndrome, who had severe impairments of control and voluntariness, whose behavior was characterized by aspontaneity and lack of correction. Let's start with examples.
The patient, who received a severe injury to the left frontal lobe, had difficulty recognizing objects drawn with a dotted line or shaded, and was unable to grasp and convey the meaning of two paintings successively depicting simple subjects (in one painting, two guys are smoking near a haystack; in the other, they are running away from a fire haystack). Patient: “Here two are sitting, and here two are running.” The patient does not notice that we are talking about a sequential image.
Doesn't it look like agnosia? But that's not true. The fact that recognition difficulties are pseudo-agnostic is indicated by the fact that as soon as you asked the patient to “look carefully” at how he gave an adequate answer. The difficulty of recognition in this case is not an agnostic disorder in the narrow sense of the word, but is a consequence of the fact that the patients did not carry out an active search process, which is always included in the act of perception.
It is especially difficult for patients with damage to the frontal lobes of the brain to understand a series of pictures depicting a plot in a sequential order. Thus, one such patient with damage to the basal parts of the frontal lobes of the brain was presented with a series of five pictures depicting a wolf chasing a boy through a snowy clearing in the forest. “Look, you’re a mischievous person, you climbed a tree to get apples or something,” says the patient, barely looking at this picture. After the experimenter's persistent request to look more closely, the patient correctly describes the plot.
Thus, the data presented show that a significant role in such disorders is played by a violation of controllability and voluntariness, i.e., the motivational component of perception suffers.
This involuntariness is manifested in another peculiar phenomenon - in such patients there is no change in figure and ground in Rubin's reversible figures. As you know, if you fix an image for a long time, the process of changing figure and background occurs by itself; otherwise, it is enough to draw the subject’s attention to the possibility of such a change in order to arbitrarily trigger this process. In the patients described, this process of changing figure and ground cannot be voluntarily caused.
Likewise, they do not form hypotheses when presented with Rorschach blots.
Let us provide two pieces of evidence that the noted disturbances in perception are personal-based.
The first (theoretical) comes from Freud.
In American psychology, the term personality denotes a certain integrative system that ensures the integrity and constancy of an individual’s behavior and which is constantly in danger of destruction either from forbidden instinctual drives or from demands imposed by the external world (dog below and dog above). The presence of such a constant conflict creates a certain level of anxiety. When it increases, psychological defense mechanisms are launched, the purpose of which is to eliminate the source of anxiety and return the individual to a state of comfort.
As an example, let us dwell on the form of psychological defense that is called perceptual. The activation of the perceptual defense mechanism is associated with the degree of structure of the perceptual material. An uncertain, conflictual or unfamiliar situation that requires a restructuring of behavioral patterns and adaptation to new relationships can lead to an increase in the level of anxiety. It is intolerance to uncertainty that causes perceptual defense (for example, denial of an obvious fact), i.e., a disorder of perception.
Second (experimental) proof according to B.V. Zeigarnik. The experimental procedure was as follows. The subjects were presented with complex plot pictures and pictures with an unclear plot under conditions of different motivation, which was created, firstly, with the help of different instructions; secondly, by varying degrees of image uncertainty.
The pictures used in the experiment were images of more or less complex situations (a mother bathing a child, a group of excited women, etc.), blurry photographs of objects (flowers, wet pavement, Rorsch blots). The difference in the instructions was as follows. In option “A,” picture cards were offered with “blind” instructions to describe what was depicted. Option B stated that the purpose of the experiment was to explore imagination. In option "B", subjects were warned that the purpose of the study was to determine their mental abilities. In each variant, different sets of pictures were presented. Thus, in all three options, the goal of the task remained unchanged, only its motivation changed.
The experiments involved healthy subjects, patients with epilepsy and patients with schizophrenia.
Healthy subjects. Under the conditions of option “A,” the perception process was not determined by the experimentally specified motivation. Because of this, the immediate goal of the activity—meaningful interpretation—did not acquire independent motivating force.
Qualitatively different results were obtained in options “B” and “C”, where the motives introduced by the instructions set a certain direction of activity.
Normally, this was expressed in the fact that the subjects became interested in the task and the experimenter’s assessment. The nature of the formulation of hypotheses has also changed - they have become more detailed and emotionally rich. The central place in the description of plot pictures began to be occupied by the disclosure of the inner world of the depicted characters. Formal answers have disappeared.
We will demonstrate the peculiarities of perception in a patient with epilepsy using the example of the patient’s statements when presented with a picture depicting a group of excited women.
“There are several people in this picture. There is a woman standing on the left, and another woman next to her. Her hair is dark, she folds her arms over her chest and cries. A boy is running towards her, raising his hands, as if he wants to calm her down... Behind the boy, a woman is holding a child or he is sitting on something, pressed against her, hugging her with his right hand... In the left corner there are two more women...", etc.
The above example shows how activity, initially aimed at a meaningful interpretation of a picture, turns into a scrupulous description of its individual fragments. In some cases, this inhibits the process of generating hypotheses, leading to the emergence of formal answers.
The perception activity of patients with schizophrenia has a different type. Despite the “intellectual” focus of the study, the patients did not show interest in the task, did not respond to the experimenter’s assessment, and did not correct their mistakes. The activity of patients is characterized by extreme convolution, the absence of search activity, so pronounced in the norm. The patients’ statements are extremely laconic, unemotional, and mostly only generally state some plot or subject content of the pictures: “Some kind of misfortune,” “The person is thinking.”
Thus, analysis of the research results in options “A”, “B” and “C” made it possible to establish the dependence of perception on motivation. With the introduction of meaning-forming motives, a new motivational structure is formed, different in normal and pathological conditions.
How do perceptual disorders manifest themselves?
The field of psychiatry is a special field of medicine that studies various mental disorders and their manifestations. This is a very specific area of human knowledge, which operates with the concepts of “disease”, “health”, “norm” and “pathology” in relation to mental state. One of the areas of work of a psychiatrist is perceptual disorders. Psychiatry considers such problems to be mental pathologies. Disorders of sensation and perception are manifested by several conditions:
- Anesthesia is manifested by an inability to perceive tactile sensations, taste and smell. Its manifestations are similar to medical anesthesia, which is caused to turn off the sensitivity of pain receptors in patients during medical interventions.
- Hyperesthesia is a sensitivity disorder caused by a seeming increase in smell, light, and sound. Very often, hyperesthesia occurs in patients who have suffered a traumatic brain injury.
- Hypoesthesia is the opposite of hyperesthesia, a change in sensitivity. Sensory perception reduces natural stimuli. Patients with depressive disorders suffer from hyposthesia, for whom the world seems dull and boring.
- Paresthesia is expressed in sensations of itching, burning, tingling, and “pins and needles” caused by impaired blood supply and innervation. Often, paresthesia occurs in the Zakharyin-Ged zones: problems of internal organs manifest themselves in the form of unpleasant, painful sensations in certain areas of the surface of the human body.
- Senestopathies are unpleasant sensations that arise inside the human body; they are difficult to describe in words; most often the patient uses vivid comparative images to talk about these sensations.
“Wrong” sensations sometimes coincide with the clinical manifestations of any disease, and not only from psychiatric practice. A competent diagnosis of a disease or condition is the basis of quality treatment.
Forms of perception impairment in various diseases
As shown above, perception disorders have different causes and different forms of manifestation. Knowledge of these features allows the psychologist to participate in making a diagnosis, and knowledge of the mechanisms of disorders - in the development and implementation of correctional programs.
With local brain lesions, two types of disorders are observed:
1. Sensory disorders (impaired sense of height, color perception, etc.). These disorders are associated with lesions at the subcortical levels of the analytical systems.
2. Complex gnostic disorders, reflecting a violation of various types of perception (perception of objects, spatial relationships). These disorders are associated with damage to the cortical areas of the brain.
In patients with neuroses and neurosis-like conditions, pain sensitivity is impaired. More often, there is not a decrease, but an increase in pain sensation, so-called “psychogenic” pain, which is also a violation of perception. When experiencing pain, a large role is played by anticipation and fear of pain, although, according to the research of B. D. Karvasarsky, there is no pain that is devoid of a material basis, even when it comes to psychogenic pain. At the same time, it is important to establish the relationship between the sensory and emotional components of the experience of pain in order to select the correct treatment: the predominance of medication or psychotherapy.
In epileptoid patients, perception is overly detailed and unproductive. We can say that they cannot see the forest for the trees.
In patients with schizophrenia, difficulties in recognizing objects are mostly associated with apatoabulic syndrome and emotional ambivalence.
With psychopathy of the excitable circle, sensitivity increases with an increase in emotional tone.
In psychopathy of the inhibitory type, rigidity and decreased sensitivity are noted, also with an increase in emotional tone.
In reactive depression, perception is impaired in different ways, and depends on the clinical picture:
a) with depressive-paranoid syndrome – affective distortion of perception;
b) in asthenic-depressive conditions - fragmented perception with difficulties concentrating and switching attention;
c) in hysterical-depressive - perception is suggestible, due to which pseudoagnosia is possible.
Pathologies of sensory cognition
Disorders of various types of sensory cognition include distortions of several processes in the human body: sensations, perceptions, ideas. And they are also usually divided into different types.
Changing sensitivity
{banner_banstat9}
Such variation is possible both downward and, conversely, upward. Human states are different and have their own scientific designations.
Mental hyperesthesia is a sharp increase in sensitivity even with minimal exposure to a stimulus. Sensations of smell, taste and light, which were previously normal, now cause discomfort and even pain.
The following manifestations are also noted:
- incontinence;
- anger;
- irritability;
This pathology of sensory cognition is associated with the development of the following diseases:
- amentia;
- oneiroid;
- hallucinosis;
- paranoid;
- neurotic syndromes;
- acute intoxication with strong drugs, drugs, alcohol;
- damage to the peripheral nervous system (if hypersthesia is observed on the skin).
Decreased sensitivity, in turn, has two types of disorders.
Mental anesthesia is a pathology of perception in the absence of a reaction from one of the analyzers:
- blindness;
- loss of sense of taste;
- immunity to odors;
- deafness;
- disappearance of the sensation of pain.
Only a slight drop in the level of sensitivity is called hypoesthesia.
Senestopathies are sensations that are difficult to define. They have no basis and no clear location; they are unpleasant and painful.
Classified as follows:
- thermal (burning or cold feeling);
- movement, movement of tissues (twisting, joining or delamination);
- tension;
- sensation of pulsation, transfusion;
- drilling and tearing, burning pain.
Most often, the patient determines the location of such sensations in the brain area. May occur in the chest as well as the abdominal cavity. Extremely rare - in the upper and lower extremities.
Children's fantasies and perceptual disorders
Child psychiatry and psychology is a special type of medicine. Children are great dreamers and inventors, and the increased reactivity of the child’s psyche and insignificant life experience do not give the child the opportunity to independently correct unreal sensations in time. That is why perception disorders in children are a special area of pedagogy, psychology and psychiatry. Visual and auditory illusions are one of the components of every person’s childhood. A scary fairy tale told at night becomes a real nightmare for the baby, hiding under the crib or in the closet. Most often, such disorders occur in the evening, affecting the child’s fatigue and drowsiness. Scary tales and stories, especially those told to a baby at night, can become the basis for the development of a neurotic state. Hallucinations occur in children most often against the background of somatic and infectious diseases as a result of increased body temperature. The age at which such disorders most often manifest is 5-7 years. Hallucinations of this nature are elementary - sparks, flashes of light, outlines or images of people, animals, and from the sounds children hear shouts, knocking, voices of birds or animals. All these visions are perceived by the child as a fairy tale.
Children of different ages can also suffer from manifestations of schizophrenia. In this case, all hallucinations acquire a complex, often ominous character. The plot of hallucinations is complex, often endangering the health or even the life of the baby. Children of older adolescence, which is 12-14 years old, are characterized by the development of taste and tactile hallucinations, the child begins to refuse previously loved foods, and his character and behavior change.
Pediatrics and child psychiatry classifies children with congenital disturbances of perception into a special group. In these cases, the child grows and learns to compensate for the lack of some sensations by enhancing the development of other sensory abilities. A classic example is that a child with congenital hearing loss has excellent vision, notices the smallest details, and pays more attention to minor details of the surrounding reality.
Perception is the basis of knowledge of the surrounding world in all its manifestations. In order to feel, a person is given six sense organs and nine types of receptors. But in addition to sensations, the information received must be transmitted to the appropriate parts of the brain, where it must undergo a process of processing and analysis, drawing up an overall picture of reality based on a complex of sensations and life experiences. The result of perception is a picture of the surrounding reality. Violations in at least one link in the chain of obtaining a picture of the world lead to a distortion of reality. Psychiatry as a field of clinical medicine studies the causes of appearance, stages of development, signs and symptoms, methods of treatment and prevention of perception disorders, both individual phenomena and components of general human health problems.