Severe depression causes
Severe depression usually occurs for two reasons: psychological and physiological.
For psychological reasons, depression can develop as a result of stress or any traumatic situation. This could be the death of a loved one or relative, physical or moral violence, a terrible disaster in which a person became a participant, and many others. Usually, after two months, the depressive state can go away, but without proper help it drags on and severe depression can develop.
A number of seemingly insignificant unpleasant life situations present in a person’s life for quite a long time can become a source of constant stress. Lack of material resources; work that doesn't bring you joy; forced living with unpleasant people; deterioration in the quality of life due to any chronic disease - all this can be attributed to a constant stressful situation.
Severe depression can develop due to frustration - a condition in which a person constantly feels that his desires are impossible to fulfill.
An existential crisis can simultaneously act as both a cause and a manifestation of depression. It is expressed in the loss of life goals, a feeling of the meaninglessness of existence, and an imbalance of harmony.
The physiological causes of depression have completely different roots. Alcohol and drug use, menopause, cerebrovascular accidents, severe fatigue, chronic diseases, lack of proper nutrition - this is just a small list of physiological disorders that can lead to severe depression. An important fact is that depression rarely develops for any one reason; often several factors lead to it. And successful treatment is only possible if all the causes of this mental disorder are taken into account.
Treatment of mood disorders
Therapy is complex. Initially, it is aimed at stopping an acute depressive and/or manic period. Depending on the symptoms and their intensity, the doctor selects the necessary medications. In most cases, treatment is carried out on an outpatient basis, but in severe situations, inpatient treatment is recommended.
After stabilization of the patient's condition, he must undergo psychotherapy. This is individual, group or family therapy. Its goal is to help a person understand the disease, as well as teach behavioral techniques to control their emotional state.
Treatment of affective disorders involves lifestyle changes, namely:
- reduction of external stress factors;
- proper nutrition;
- adequate activity;
- avoid mental or physical stress;
- exclusion of alcohol and other toxic substances.
After the main treatment, maintenance therapy for affective disorders is recommended. It is aimed at maintaining a long period of remission and preventing relapses.
Treatment may take several months, but if you consult a doctor in a timely manner, the prognosis is favorable.
Severe depression symptoms
The fact that a person is severely depressed is determined by the following symptoms: depressed mood, decreased performance and activity, constant feeling of fatigue, inability to concentrate on anything, constant self-flagellation and guilt, low self-esteem, thoughts of suicide, a gloomy and hopeless look for your future, insomnia or, conversely, severe drowsiness, loss of appetite.
The clinical picture of severe depression is as follows: a person experiences a persistent feeling of melancholy every day; his mood is depressive; signs of psychomotor retardation are observed; he cannot concentrate his attention on anything; sexual desire decreases; in the morning the patient feels tired and exhausted due to the fact that he cannot sleep normally at night. Manifestations of severe depression also include a feeling of suffocation and discomfort in the chest, complete apathy, pessimistic views of one’s future (a person always expects an accident to happen), lack of will, inability to make any decisions, constant drowsiness and a feeling of laziness.
Severe depression signs
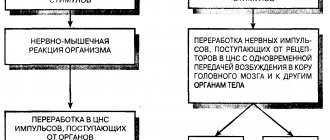
If a person does not have the strength and desire to do anything, if he cannot force himself to do anything, and at the same time is constantly in a bad, depressed mood, then this indicates signs of a depressive state. Manifestations of depression also include constant laziness, which disguises apathy. The fact is that during severe depression, a person’s brain begins to work differently - its biochemical processes change, which leads to laziness. There are three main brain transmitters that are responsible for a person’s mood, energy and performance - dopamine, norepinephrine and serotonin. And when their work is disrupted, complete apathy sets in and there is a lack of energy to engage in any activity. In such cases, it is necessary to start treatment with special drugs on time, otherwise the person simply will not want to get out of bed in the morning and will completely lose interest in life. The consequences of severe depression can be very serious and negative for the patient - a constant feeling of fear and anxiety develops, eventually acquiring manic forms.
The course of severe depression in pregnant women deserves special attention. Since it often causes miscarriage. Therefore, at the slightest sign of depression, a woman needs to seek help from a specialist.
Cognitive and affective disorders in post-stroke patients and the possibilities of their correction
T.S. MISHCHENKO, L.F. SHESTOPALOVA, V.N. MISHCHENKO Institute of Neurology, Psychiatry and Narcology of the Academy of Medical Sciences of Ukraine
Cerebral stroke is currently one of the main causes of mortality and disability in the world population [1, 2]. Every year, about 15 million strokes occur in the world and more than 6 million people die as a result of it [3, 4]. This problem is also relevant in Ukraine, where about 100–110 thousand new cases of stroke occur annually, and disability after stroke is 3.2 per 10,000 population, ranking 1st among the causes of primary disability in the country [5]. Restoring previous ability to work after a stroke is problematic for most people. Only 10–20% return to work after a stroke. From 20 to 43% require outside care, 33–48% experience hemiparesis, and 18–27% have speech disorders [1, 2, 6, 7].
Restoration of impaired functions occurs differently in each patient, which requires an individual approach to rehabilitation measures [8].
When drawing up individual rehabilitation therapy programs for post-stroke patients, it is of great importance to take into account the factors that determine the prognosis of the course of the post-stroke period of cerebral stroke, and, consequently, the effectiveness of rehabilitation [9].
There are many factors known that influence the restoration of impaired functions in post-stroke patients [9–11]. These are the age of the patients, the location and size of the lesion, the severity of the stroke, the presence of previous and concomitant diseases, early initiation of treatment and rehabilitation measures, and others [2, 11, 12]. A search for new factors is currently underway.
In recent years, a lot of convincing data have appeared indicating the influence of cognitive impairment and depressive disorders on the rate of recovery of impaired functions in post-stroke patients [13–17].
Cognitive impairment, in particular its most severe form, dementia, is a common outcome of ischemic stroke (IS). As studies have shown, they increase the degree of disability of patients and significantly complicate the process of rehabilitation of patients [18, 19]. Cognitive disorders occur after all subtypes of IS, but especially often after lacunar stroke [20, 21]. A comparative analysis of risk factors for the development of IS with cognitive impairment showed that the latter more often develop in patients with arterial hypertension, atrial fibrillation and diabetes mellitus [22, 23].
Dementia, as the most severe form of cognitive deficit, occurs in 9–36% of cases within 1–3 years after a stroke [24, 25]. Numerous studies have shown that the risk of developing dementia is 2 times higher in elderly patients who have suffered a stroke than in people of the same age, but without a stroke [26, 27]. Dementia also almost doubles the risk of mortality in post-stroke patients [28] and significantly affects the rate of recovery of functions impaired due to IS.
Why do cognitive disorders occur so often in post-stroke patients? Several reasons can be identified.
The leading role in the development of cognitive deficit is played by damage to the deep parts of the white matter of the brain and the basal ganglia, which occurs as a result of structural damage to the brain. This leads to disruption of the connection between the frontal lobes of the brain and subcortical structures (disconnection phenomenon) [29, 30].
In addition to damage to deep cerebral structures and the occurrence of the phenomenon of disconnection with secondary dysfunction of the frontal parts of the brain, cerebral infarctions of the cortical localization play an undoubted role in the pathogenesis of cognitive impairment [31].
An equally important aspect of the pathogenesis of cognitive disorders in patients who have suffered a stroke is the addition of a neurodegenerative process. According to pathomorphological data, the coexistence of vascular changes and markers of Alzheimer's neurodegeneration (senile amyloid plaques, neurofibrillary intracellular tangles, apoptosis of neurons in the mediabasal frontal regions, hippocampus and temporo-parietal lobes of the brain) is not rare [32]. In these cases, it is customary to talk about the mixed vascular-degenerative nature of dementia.
Thus, cognitive impairment in post-stroke patients has a complex pathogenetic mechanism of development.
In addition, affective disorders have a significant impact on the rate of recovery of impaired functions. The latter include depression, anxiety, apathy, emotional lability, and mania. Post-stroke depression (PD) in frequency far exceeds other affective disorders, which explains the increased attention to this problem for many years [33–36]. The frequency of depression, according to various authors, varies from 6 to 60%, averaging 20–30% [37–40]. The presence of depression increases mortality by 2.6 times and also has a negative impact on the rehabilitation process [41, 42].
For many years, PD was interpreted as a patient’s emotional reaction to an illness. However, it was later found that social, personal and other factors take part in the formation of depressive symptoms. Such factors include age, gender, severity and location of stroke, the degree of disability of the patient, his premorbid personality characteristics, the presence of cognitive impairment, living alone, etc.
Thus, cognitive impairment and depression are common outcomes of IS and significantly affect mortality and the rate of recovery of impaired neurological functions. Therefore, identification and correction of such disorders are an important part of rehabilitation measures for post-stroke patients.
An important place in the treatment of post-stroke patients is occupied by the search for drugs that would affect both cognitive and affective disorders. This makes it possible to reduce the number of medications prescribed to patients in the post-stroke period. As a rule, patients who have undergone IS should receive antihypertensive, lipid-lowering, and antiplatelet therapy. Prescribing drugs with multiple mechanisms of action can reduce the number of side effects of therapy, as well as the cost of treatment.
In this context, it was of interest to study the possibilities and effectiveness of using the drug Pramistar, which recently appeared on the pharmacological market of Ukraine, in post-stroke patients.
The choice of drug used was determined by the unique mechanism of action of Pramistar (pramiracetam).
Pramistar inhibits brain neuropeptidases, leading to the accumulation of peptides involved in the formation of long-term memory. It stimulates the high affinity choline uptake system and accelerates acetylcholine synthesis. Acetylcholine, in turn, triggers the activity of nitric oxide synthetase.
Nitric oxide plays an important role in learning and memory, especially in the formation of short-term memory. Pramiracetam also has antidepressant effects, potentiating the effects of methamphetamine [43–45].
Thus, the pharmacodynamics of pramiracetam are based on three experimental findings: activation of the choline uptake system, inhibition of neuropeptidases and potentiation of amphetamine action.
Thanks to its triple mechanism of action, Pramistar has proven effective in numerous double-blind, controlled and open-label studies in the treatment of patients with Alzheimer's disease [45]. Improvements in general learning ability (based on the MMSE scale), verbal function, and concentration have been demonstrated in these patients.
The effectiveness, safety and good tolerability of Pramistar have been proven in numerous double-blind, placebo-controlled and open studies. It is these properties of the drug Pramistar that determined its choice for the treatment of patients who have severe cognitive impairment and depressive disorders.
To solve the research problem, a clinical-neurological method was used in the work. The Rankin scale was used to assess the functional abilities of patients. To objectify the state of cognitive functions, the Mini-Mental State Examination (MMSE) scale was used [46]. To assess voluntary attention, the Schulte table method was used. The Beck and Hamilton scales were used to assess depressive disorders.
A psychodiagnostic study was carried out three times: the first study (background) - before starting to take the drug (day 0), the second - after 4 weeks of taking the drug (mid-course), the third - after 8 weeks of taking the drug.
64 patients (34 men and 30 women) aged from 56 to 72 years (mean age 60.2 ± 1.2 years), 3–6 months after ischemic stroke, were examined. In 23 patients, the lesion was localized in the right system, in 21 - in the left internal carotid artery, and in 20 patients - in the vertebrobasilar system.
The criterion for inclusion in this study was the presence of cognitive impairment and depressive syndrome in the clinical picture of the disease. The study did not include patients with severe aphasic disorders and severe disability (4 points or more on the Rankin scale), or with kidney pathology.
Patients received Pramistar at a dose of 1 tablet (600 mg pramiracetam sulfate) 2 times a day for 2 months. Treatment was carried out against the background of therapy that forms the basis of secondary prevention, namely antihypertensive and antiplatelet therapy.
Efficacy, tolerability and safety were assessed after 1 and 2 months from the start of therapy.
The clinical picture of the disease in the patients we examined was determined to be a combination of neurological deficits, cognitive impairment, and depressive disorders.
We assessed the neurological status of the examined patients before and after treatment.
Patients complained of headaches, dizziness, weakness in the limbs, decreased memory and attention, tearfulness, irritability, a feeling of constant fatigue, and disturbed night sleep. A month after the start of treatment, most patients noted a decrease in headaches, dizziness, noise and a feeling of heaviness in the head, irritability, lethargy, and improved night sleep.
By the end of the study, a more pronounced regression of the above symptoms of the disease was observed. After just 1 month of treatment, the vast majority of patients noted an improvement in well-being, a slight increase in the level of mental performance, improved concentration, an increase in mood and general level of activity. Patients became more active and better involved in the rehabilitation process.
After 2 months of treatment, a more pronounced increase in the overall level of activity, improvement in memory, and attention was observed.
As evidenced by the data, all the patients we examined had clear cognitive impairments that reached the degree of clinically significant cognitive decline, and in 24% of patients - the degree of dementia. The structure of cognitive dysfunction was dominated by disorders of verbal memory (2.3 ± 0.4 points), counting operations (1.6 ± 0.4 points), and gnostic functions (5.9 ± 0.8 points). The overall cognitive productivity score was 17.3 ± 1.7 points.
In the middle of the course of treatment, patients showed an improvement in orientation functions (respectively 7.5 ± 0.4 points before treatment and 8.3 ± 0.3 points after treatment, p ≤ 0.05) and verbal memory (2.3 ± 0. 4 and 2.7 ± 0.5 points, the differences are not significant).
After 8 weeks of therapy, there was a clear improvement in all assessed cognitive functions. The overall cognitive productivity of patients significantly increased (21.4 ± 1.8 points, p ≤ 0.05 compared to the background study).
There was a statistically significant improvement in the functions of verbal memory (3.4 ± 0.7 points), orientation (8.8 ± 0.6 points), and perceptual-gnostic operations (7.2 ± 1.1 points).
A study of the dynamics of voluntary attention functions during Pramistar therapy in patients who suffered an ischemic stroke showed the following.
As evidenced by the data in Table. 2, the examined patients showed a statistically significant decrease in the time required to complete the task for each of the 5 Schulte tables already by the middle of the treatment course, i.e. parameters such as volumes of voluntary attention, functions of its concentration, distribution and switching were improved. The indicator of overall work efficiency increased, but the performance indicators remained low.
During further treatment with Pramistar, the functions of voluntary attention continued to significantly improve, while the indicator of processing ability also increased. Thus, in the examined patients, indicators of attention functions steadily increased throughout the entire treatment with the drug, which indicates a certain restoration of voluntary attention operations and mental performance in general.
To assess the effect of the drug Pramistar on depressive disorders in patients who had suffered a cerebral stroke, we used indicators of the Beck and Hamilton scales.
As evidenced by the data, the patients we examined before treatment had mild to moderate depressive experiences, as evidenced by the indicators of the Beck and Hamilton scales.
After 8 weeks of therapy with Pramistar, there was a statistically significant decrease in Beck scale scores (20.2 ± 5.9 and 9.5 ± 4.3 points, respectively, p ≤ 0.05), which corresponded to both the subjective self-reports of patients and results of clinical examination.
After 2 months of taking Pramistar, there was an improvement in the well-being of patients, sleep normalized, anxiety and general weakness decreased, and mood levels increased.
All patients we examined tolerated the drug well; no side effects were observed.
Thus, after monotherapy with Pramistar, there was an improvement in the neurological status, cognitive functions and a decrease in depressive disorders in post-stroke patients. There was a decrease in the severity of headaches, dizziness, and an increase in the general activity of patients.
In addition, an increase in the volume and strength of voluntary verbal memory, the volume of voluntary attention, an improvement in the process of learning and the level of mental performance were noted. There was an improvement in mood, quality of self-care, and orderliness in behavior.
Thus, patients receiving Pramistar for 8 weeks showed a clear improvement in basic cognitive functions: improvement in verbal memory functions in the form of an increase in the volume of immediate memory and long-term memory; improving the functions of voluntary attention, increasing the volume of processed information, reducing the phenomena of exhaustion, improving speed parameters; reduction in the severity of perceptual-gnostic disorders; general increase in cognitive productivity of patients; reduction of depressive experiences and asthenic symptoms.
All this has made it possible to increase the effectiveness of rehabilitation measures and improve the quality of life not only of post-stroke patients, but also of people caring for them. Pramistar reduces the severity of neurological manifestations of the disease, has a positive effect on all basic cognitive functions, and also helps reduce depressive symptoms.
The results of the study allow us to recommend the inclusion of the drug Pramistar in the complex treatment of patients who have suffered IS.
Literature 1. Wiebers D., Feigin V., Brown R. Guide to cerebrovascular diseases. - M.: ZAO "Publishing House BINOM", 1999. - 672 p. 2. Worlow C.P., Dennis M.S., Gein J. et al. Stroke. Practical guide for the management of patients. - St. Petersburg: Politekhnika, 1998. - 629 p. 3. Adams HP, Adams RJ, Brott T, Del Zoppo GJ et al. Guidelines for the early management of patients with ischemic stroke. A scientific statement from the stroke council of the American stroke association // Stroke. - 2003. - V. 34. - P. 1056-1083. 4. Wolf CDA, Giroud M., Kolomisnky-Rabas P. et al. Variations in stroke incidence and survival in 3 areas of Europe // Stroke. - 2000. - V. 31. - P. 2074-2079. 5. Voloshin P.V., Taitslin V.I. Treatment of vascular diseases of the brain and spinal cord. - M.: MEDpress-inform, 2005. - 688 p. 6. Chalmers J., Chapman N. Progress in reducing the burden of stroke // Clin. Exp. Pharmacol. Physiol. - 2001. - V. 28. - P. 1091-1095. 7. Vanelay F. Functional outcome measures in stroke rehabilitation // Stroke. - 1991. - V. 22. - P. 105-108. 8. Belova A.N., Shchepetova O.N. Guidelines for the rehabilitation of patients with movement disorders. - M.: Medicine, 1998. - P. 30-33. 9. Gusev E.I., Gekht A.B., Bogolepov A.N., Sorokina I.B. Features of depressive syndrome in patients who have suffered an ischemic stroke // Journal of Neurology and Psychiatry. Stroke application. - 2001. - Issue. 3. - pp. 28-31. 10. Gusev E.I., Skvortsova V.I. Cerebral ischemia. - M.: Medicine, 2001. - 327 p. 11. Deev A.S., Zakharushkina I.V. Causal factors, course and outcomes of ischemic stroke in young people // Nevrol. magazine. - 1999. - No. 6. - P. 28-30. 12. Demidenko T.D., Ermakova N.G. Fundamentals of rehabilitation of neurological patients. - St. Petersburg: Foliant, 2004. - 304 p. 13. Gekht A.B., Bogolepova A.N., Sorokina I.B. Features of depressive syndrome in patients who have suffered an ischemic stroke // Journal of Neurology and Psychiatry named after. S.S. Korsakov. - 2001. - Issue. 2. - pp. 35-39. 14. Maruta N.A., Moroz V.V. Neurotic depression (clinic, pathogenesis, dynamics and treatment). - Kharkov: Aris, 2002. - 144 p. 15. Podkorytov V.S., Chaika Yu.Yu. Depression. Modern therapy. - Kharkov: Tornado, 2003. - 349 p. 16. Morin M., Barda R., del Ser T. et al. Dementia is a risk factor for mortality in stroke patients // Cerebrovasc. Dis. - 2002. - V. 13 (Suppl. 3). - P. 68. 17. Paolucci S., Antonucci G., Grasso MG et al. Post-stroke depression, antidepressant treatment and rehabilitation results: a case-control study // Cerebrovasc. Dis. - 2001. - V. 12. - P. 264-271. 18. Yakhno N.N., Zakharov V.N. Mild cognitive impairment in old age // Neurological Journal. - 2004. - No. 1. - P. 4-8. 19. Vilensky B.S., Semenova G.M. Cause of death due to stroke and possible measures to reduce mortality (clinical and pathological study) // Nevrol. magazine. - 2000. - T. 5, No. 4. - P. 10-13. 20. Boiten J., Lodder J. Lacunar infarcts // Stroke. - 1991. - V. 22, No. 8. - P. 1374-1378. 21. Bowler JV Vascular cognitive impairment // Stroke. - 2004. - V. 35. - P. 386-388. 22. Patel M., Coshall C., Rudd A., Wolfe C. Natural history of cognitive impairment after stroke and factors associated with its recovery. Cerebrovasc. Dis. - 2001. - V. 1 (Suppl. 4). — P. 9 23. Sacco RL Risk factors, outcomes, and stroke subtypes for ischemic stroke // Neurology. - 1997. - V. 49. - P. 39-44. 24. Ghika-Schmid F., Van Melle G., Guex P. et al. Subjective experience and behavior in acute stroke: the lausanne emotion in acute stroke study // Neurology. - 1999. - V. 52. - P. 22-28. 25. Hoehstenbaeh JB, den Otter R., Mulder TW Cognitive recovery after stroke: a 2-year follow-up // Arch. Phys. Med. Rehabil. - 2003. - V. 84 (10). — P. 1499-1504. 26. Desmond DW, Moroney JT, Paik MC et al. Frequency and clinical determinants of dementia after ischemic stroke // Neurology. - 2000. - V. 54. - P. 1124-1131. 27. Voisin T., Rous de Feneyrols A., Pavy Le Traon A., Larrue V. Cognitive impairment after first lacunar stroke: clinical features and risk factors // Cerebrovasc. Dis. - 2002. - V. 13 (Suppl. 3). — P. 69 28. Henon H., Durieu I., Godefroy O. et al. Influence of dementia on mortality in stroke patients: a 30 year // Cerebrovasc. Dis. - 2000. - V. 10 (Suppl. 2). - P. 87 29. Yakhno N.N., Damulin I.V., Zakharov V.V. Memory impairments in neurological practice // Neurological Journal. - 1997. - No. 4. - P. 4-9. 30. Bowler JV Vascular cognitive impairment // Stroke. - 2004. - V. 35. - P. 386-388. 31. Voloshina N.P. Dementing processes of the brain. - Kharkov: Osnova, 2001. - 187 p. 32. Vilensky B.S. Stroke: prevention, diagnosis and treatment. - St. Petersburg, 1999. - P. 336. 33. Depression in neurological practice (clinic, dynamics, treatment) / Wayne A.M., Voznesenskaya T.G., Golubev V.L. and others - M.: Medical Information Agency, 2002. - 160 p. 34. Kataev N.G., Kornetov N.A., Kataev S.G., Levina A.Yu. Clinical and laboratory dynamics of organic and depressive mental disorders in post-stroke patients // Russian Psychiatric Journal. - 2005. - Issue. 4. - pp. 9-12. 35. Mishchenko V.N. Post-stroke depression // Journal of psychiatry and medical psychology. - 2004. - No. 2 (12). — P. 81-83. 36. Savina M.A. Post-stroke depression // Journal of Neurology and Psychiatry. - 2005. - No. 7. - P. 67-74. 37. Palomaki H., Kaste M., Berg A. et al. Prevention of poststroke depression: 1 year randomized placebo controlled double blind trial of mianserin with 6 months follow up after therapy // J. Neurol. Ncurosurg. Psychiat. - I999. - V. 66. - P. 490-494. 38. Pantoni L., Martini M., Bartolini L. et al. Diagnosis of major depression in subcortical vascular encephalopathy // Cerebrovasc. Dis. - 2003. - V. 16 (Suppl. 4). - P. 43 39. Paolucci S., Antonucci G., Grasso MG et al. Post-stroke depression, antidepressant treatment and rehabilitation results: a case-control study // Cerebrovasc. Dis. - 2001. - V. 12. - P. 264-271. 40. Paradiso S., Robinson RG Gender differences in post-stroke depression // J. Neuropsychiatry Clin. Neurosci. - 1998. - V. 10. - P. 41-47. 41. Piccinelli M., Wilkinson G. Gender differences in depression: critical review // Br. J. Psychiat. - 2000. - V. 177. - P. 486-492. 42. Pohjiasvaara T., Leppavuori A., Siira I. et al. Frequency and clinical determinants of poststroke depression // Stroke. - 1998. - V. 29. - P. 2311-2317. 43. Burchinsky S.G. Metabolic strategy in the treatment of cerebral ischemia // Faces of Ukraine. - 2005. - No. 10. - P. 82-83. 44. Funk KF et al. Zur cholinergen wirkung von nootropika // Biomed. Biochim. Acta. - 1988. - V. 47. - P. 417-421. 45. Pugsley T. A . et al. Some neurochemical properties of pramiracetam, a new cognition-enhancing agent // Drug Development Research. - 1983. - V. 3. - P. 407-420. 46. Folstein MF, Folstein SE, McHugh PR Mini-mental State: a practical method for grading the cognitive state of patients for the clinicians // J. Psychiat. Res. - 1975. - V. 12. - P. 189-198.
Severe depression and suicide
Severe depression is dangerous because the patient completely loses the instinct of self-preservation. A persistent feeling of melancholy, as well as constant pain tormenting his soul, makes him think about suicide. An overwhelming feeling of guilt, a feeling that he deserves punishment, a desire to free his loved ones, often push a person to commit suicide. According to statistics, 15% of people with mental disorders of unknown etymology become victims of suicide.
At the onset of the disease, the person is so weak, exhausted by severe depression, that he is unable to take any steps to take his own life. But as soon as this condition goes away, the patient may attempt to commit suicide. He will think through the suicide plan in detail, develop it, and try to create a deceptive impression that he has gotten better, without leaving the thought of committing suicide.
The most common cases of suicide are among lonely people with a history of somatic illnesses and people with a history of suicide in their family.
What should a person do if he has all the signs of severe depression? There is only one answer to this question: seek help immediately. If depression is not treated, it will become chronic, and this is fraught with very dangerous consequences.
Diagnostics
If signs of depressive disorder appear, you should consult a psychotherapist. To diagnose the disease, the Zang, Beck or Hamilton scale is used. With their help, it is possible to determine the severity and severity of depressive disorder. Laboratory tests are not used for depression, so it is not possible to identify which of the mediators causes the disorder.
In diagnosing the disease, a differential method is used regarding:
- mood disorders that are provoked by organic disorders of the brain;
- schizophrenic and bipolar disorders.