Catatonic stupor is a state of psychomotor immobility and behavioral disturbances manifested by stupor. It was first described in 1874 by Carl Ludwig Kahlbaum in German: Die Katatonie oder das Spannungsirresein (Catatonia or Tension Insanity).
Although catatonia has historically been associated with schizophrenia (catatonic schizophrenia), it is now known that catatonic symptoms are nonspecific and can be observed in other mental disorders and neurological conditions. The fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM) does not recognize catatonia as a separate disorder, but is associated with psychiatric conditions such as schizophrenia (catatonic type), bipolar disorder, post-traumatic stress disorder, depression and other mental disorders, narcolepsy, and also drug abuse or overdose (or both). It may also occur in many medical disorders, including infections (such as encephalitis), autoimmune disorders, focal neurological lesions (including strokes), metabolic disorders, alcohol withdrawal, and abrupt or too rapid benzodiazepine withdrawal. The fifth edition of the DSM states that various medical conditions can cause catatonia, especially neurological conditions: encephalitis, cerebrovascular disease, neoplasms, head trauma. In addition, metabolic conditions: homocystinuria, diabetic ketoacidosis, hepatic encephalopathy, hypercalcemia.
This may be an adverse reaction to prescribed medications. This has similarities to conditions such as encephalitis lethargica and neuroleptic malignant syndrome. There are many treatments available; Benzodiazepines are the first-line treatment strategy. Electroconvulsive therapy is also sometimes used. There is growing evidence of the effectiveness of NMDA receptor antagonists in benzodiazepine-resistant catatonia. Antipsychotics are sometimes used but require caution because they can worsen symptoms and have serious side effects.
Causes of stupor
Possible causes of stupor include:
- mental illness;
- diseases of the nervous system.
This condition can be a consequence of severe depression and prolonged psychosis, neuroses, and schizophrenia. It also develops as a result of encephalopathies and brain damage due to infectious diseases, intoxication and trauma.
Impressionable and emotionally unstable people often fall into a stupor after they experience some kind of shock or become witnesses or participants in emergency incidents.
Note! Knowing the reasons for the development of stupor, you can reduce the likelihood of developing this condition to a minimum. To do this, it is necessary to avoid stress and situations that traumatize the psyche, as well as promptly treat mental and neurological diseases
Treatment of catatonic stupor
Initial treatment is aimed at relieving symptoms. Benzodiazepines are the first line of treatment and high doses are often required. A test dose of intramuscular lorazepam often results in noticeable improvement within half an hour. In France, zolpidem has also been used in diagnosis, and response may occur within the same time period. Ultimately, the root cause needs to be treated. Electroconvulsive therapy (ECT) is an effective treatment for catatonia, but it has been noted that additional high-quality randomized controlled trials are needed to evaluate the effectiveness, tolerability, and protocols of ECT for catatonia.
Antipsychotics should be used with caution because they may worsen catatonia and are a cause of neuroleptic malignant syndrome, a dangerous condition that can mimic catatonia and requires immediate cessation of the antipsychotic. Excessive glutamate activity is thought to be associated with catatonia; when first-line treatment options fail, NMDA antagonists such as amantadine or memantine are used. Amantadine may have increased tolerance with long-term use and may cause psychosis due to its additive effects on the dopamine system. Memantine has a more targeted pharmacological profile to the glutamate system, reduces the incidence of psychosis and may therefore be preferable for people who cannot tolerate amantadine. Topiramate is another treatment option for refractory catatonia; it produces its therapeutic effects by causing glutamate antagonism through modulation of AMPA receptors. Treatment modalities include pharmacotherapy and electroconvulsive treatment (ECT). Prompt treatment in the early stages of catatonic states is critical to achieve long-term relief of symptoms. Treatable conditions must be identified immediately. In particular, neuroleptic malignant syndrome (NMS), encephalitis, including anti-NMDA receptor encephalitis, nonconvulsive status epilepticus, and acute psychosis must be diagnosed and treated. Although BZPs are extremely safe medications when used in the short term, when There are several issues to consider in the treatment of BZD. These include (1) the risk of hypoventilation in obese patients or patients with obstructive sleep apnea, (2) falling in elderly patients or patients with balance problems once they begin to move after resolution of their catatonia, and (3) the potential for and small, for previously immobile patients to develop into a more agitated form of catatonia. Once the catatonic state is successfully treated and patients become more active, physical and psychiatric examinations and additional investigations may be performed as needed. Surgery usually eliminates the need for interventions such as intravenous hydration and catheterization because patients begin eating and drinking almost immediately. Psychiatric diagnoses are now classified on a syndromic basis. Catatonia syndrome, however, remains in diagnostic uncertainty, recognized predominantly as a subtype of schizophrenia. However, catatonia is present in approximately 10% of acute psychiatric patients, only a small number of whom have schizophrenia. Among patients with comorbid mood disorders, which constitute the largest subgroup of patients with catatonic illness, catatonic symptoms usually resolve abruptly and completely with benzodiazepine therapy.
Causes
There are many similarities and many differences between psychiatric and general stupor: their clinical picture seems very similar, but the cause and outcomes can be completely different.
In psychiatry, stupor develops as one of the types of mental disorders; its development can be caused by:
- stressful situations;
- psychotraumatic situations;
- diseases of the nervous system;
- character traits.
Most often, such a condition as stupor develops in people who are emotionally unstable, impressionable, prone to exaggerating events, who have experienced severe nervous shock, or who have become a participant or witness to some frightening events (catastrophe, accident, violence). A stuporous state can develop in people with diseases of the nervous system, depression, schizophrenia or neurosis.
Damage to brain cells during trauma, severe infectious diseases, and intoxication causes a cascade of reactions that successively causes stupor, stupor, and coma.
These stages of impaired consciousness differ from each other in the severity of the patient’s condition. So, with a disorder such as stupor, the patient reacts to strong stimuli, with certain efforts comes into contact with others and performs some actions.
With stupor, the reaction only to painful stimuli persists; it is almost impossible to get out of this state on your own, and if the patient is not given help, his condition will worsen and he will develop a coma. Coma is a severe disorder of consciousness in which the patient does not respond to external stimuli, including pain. This condition is considered borderline and it is impossible to bring the patient back to life without intensive medical care.
Stupor-stupor-coma in intensive care practice
In resuscitation, stupor is one of the emergency conditions with depression of consciousness preceding stupor and coma.
The differences between stuporous, soporous and comatose states manifest themselves in the depth of the patient’s disturbance of consciousness:
- Stupor : drowsiness, disorientation in place and time are noted. The condition resembles alcohol intoxication, the reaction to external irritations is reduced. The patient answers questions slowly and sluggishly, often immediately falling asleep and falling into a stupor.
- Stupor : the patient is unconscious, reacts only to strong stimuli (prick, shout, shaking), responding with purposeful actions. The condition resembles deep sleep.
- Superficial coma : the patient is unconscious and responds to strong painful stimuli with erratic actions.
- Deep coma : the patient is unconscious, there is no reaction to any external stimuli.
Stupor, stupor or coma can occur due to a number of diseases, such as infections of the brain and its membranes, acute cerebrovascular accidents, diabetes mellitus, liver and kidney diseases, severe traumatic brain injuries, acute poisoning, overdose of drugs, alcohol, some medicines, etc.
As a result, the state of stupor can occur in the practice of doctors of various specializations: neurologists, infectious disease specialists, endocrinologists, general practitioners, etc.
Causes of stuporous state
If we consider all the underlying causes of stupor, we can conclude: this is nothing more than capitulation to danger. Scientists believe that it is human nature to respond to danger in one of two possible ways, namely:
- Fight.
- Run.
Often danger leaves us no time to think (otherwise we would try to avoid it) and our subconscious mind independently and instantly sends a signal to our body exactly what it needs to do. But there are situations when neither flight nor fight will help; the simplest example is a passenger in a falling plane.
Stupor is a sentence that an individual has passed on himself. The body capitulates to a danger that can neither be avoided nor reduced, and it is the experience of fatal helplessness that causes this state.
But it happens that a person falls into a stupor, as they say, out of nowhere. The situation that led to it is neither particularly traumatic for the psyche nor dangerous for physical health. Here past experience can play a cruel joke on us.
In any situation, a person makes a decision on how to act in a given situation, guided by:
- intuition;
- your feelings;
- based on past experience.
Moreover, this decision is often made unconsciously and many times a day, automatically and instantly.
will fall into a stupor.
This is, of course, a joke, but it perfectly demonstrates that in those cases when we acted in a situation familiar to us and received a result that did not correspond to our past experience, we end up with stupor. Although not something that deserves hospitalization or an urgent visit to a psychiatrist, it is also a stuporous state.
Types of stupor and its symptoms
Before moving on, let's take a quick look at the types of stupor and give them a very brief description. So, there is a stupor:
- Akinetic. This condition is characterized by maintaining the body position in one position for a long time and resisting its change.
- Apathetic. It is characterized by a lack of motivation for any activity, both motor and mental, disorientation, and paucity of experiences.
- Affective, depressive, melancholic stupor. It is observed with deep depression and is usually accompanied by a mournful expression on the face and posture.
- Hallucinatory or hallucinatory-paranoid stupor is accompanied by hallucinations, either auditory or visual.
- Catatonic. It is a manifestation of catatonic syndrome and is characterized by passive negativism or waxy flexibility, and in the most extreme manifestation – muscle numbness in the fetal position.
- Manic. Combined with the patient's extremely agitated mood.
- Negativistic. In this state, the patient is in a daze, but resists attempts at external influence.
- Effective or empty. There are no other psychopathological disorders.
There are conditions that are clearly caused by traumatic experiences:
- Hysterical, psychogenic, pseudocatatonic, emotional stupor occurs as a result of severe mental trauma, for example, the loss of a loved one, being in a war zone, captivity, rape.
- Post-shock. Occurs after a natural or man-made disaster: fire, tsunami, car accident, etc.
Stupor can be a symptom or consequence of a mental illness or severe brain damage, either organic, chemical or infectious:
- Receptor. Occurs against the background of schizophrenic delirium.
- Exogenous. This condition occurs against the background of toxic or infectious damage to the brain.
- Epileptic. Brief stupor lasting from several hours to several days in epileptics.
- Stupor, apparent or Westphalian pseudostupor, occurs against the background of severe mental disorders and is directly associated with them.
Stupor in psychiatry
In contrast to the above, various forms of blockage encountered in psychiatry do not arise as a result of the general serious condition of the patient, but are a consequence of psychopathological processes and diseases. Stupor in psychiatry is considered as a movement disorder, consisting of inhibition of motor and speech activity, without any attempts on the part of the patient to overcome this condition.
The reasons leading to the occurrence of such a condition can be organic (schizophrenia, epilepsy, acute psychosis, intoxication, damage to brain structures) or functional (stress, emotional shock, depression, prolonged fear, hysteria, apathy, etc.).
However, the specific biochemical and neurophysiological mechanisms of stupor have not been sufficiently studied to date. It is assumed that it can occur against the background of a deficiency of gamma-aminobutyric acid in the structures of the brain, with a sharp lack of dopamine in the body and some other processes.
Motor retardation during stupor can manifest itself in varying degrees - from moderate limitation in movements to complete immobility. Stupor is also characterized by mutism - partial or complete absence of speech activity.
The patient makes no attempts to get out of this state, and there is no volitional direction in his actions. The duration of stupor can range from a few minutes or hours to many months.
Signs of a soporous state
- A person with stupor seems to be sleeping, but may have some reaction to a strong irritant. If a sharp sound occurs, the patient’s eyes react – they open, but do not look for the source.
- If you press on the nail, the patient will withdraw his hand. A strong negative reaction may occur to the injection, but it is quite short-lived. The patient may even begin to swear or fight.
- If you conduct a general examination, you will notice decreased muscle tone and suppressed deep reflexes. There may be pyramidal signs due to decreased central motor neuron input.
- Focal neurological symptoms may also be observed in parallel, which will indicate local damage to structures and areas of the brain.
- If the stuporous state was provoked by hemorrhage inside the skull, then stiffness of the neck muscles and other meningeal symptoms will be noted. There may also be cramps and muscle twitching. Read more about the symptoms and treatment of cerebral hemorrhage.
- The patient may also experience hyperkinetic stupor - the patient mutters something to himself, makes unfocused movements.
Level of consciousness during stupor
As for the consciousness in such a situation, the patient is quite cloudy, and he is not able to answer any questions, the reaction is short-lived even to strong stimuli.
Symptoms of stupor
It is often difficult to determine the state of a dissociative disorder by external signs; examination with specialized equipment and hospital stay are necessary.
Doctors monitor the patient’s pulse and breathing, indicators during sleep and wakefulness, also summarize all the results and come to a final diagnosis. A symptom of such a pathology may be an inadequate reaction to an external stimulus, noise, light, pain, etc.
Symptoms of dissociative stupor:
- the patient freezes and does not respond to external stimuli;
- lack of speech and feedback;
- there are no spontaneous movements;
- impaired eye coordination;
- inadequate reaction to touch and pain.
Only thanks to specialized equipment can it be determined that a person is awake and understands where he is and what is happening to him.
With emotional or psychogenic stupor, the patient looks inhibited and may have affective tension.
Types of catatonia
Two different manifestations of motor activity disorders are observed in this condition:
- catatonic stupor;
- catatonic excitement.
Catatonic stupor
Stupor occurs due to a traumatic mental event. Stupor, along with amnesia, identity disorder, derealization, depersonalization and other pathologies, is included in the group of dissociative disorders. These conditions develop after severe stressful situations and are accompanied by clouding of reason and the development of other psychopathological processes.
A short-term stupor can last for seconds, and this state occurs quite often; in everyday situations, many freeze in place from horror. Such short-term catatonic stupor does not require treatment. Longer-term motor activity disorders are considered to be quite rare deviations. Dissociative disorders occur during natural disasters, industrial disasters and other extensive destruction. Movement disorders are treated by psychiatrists, who should be contacted in such cases.
Catatonic stupor is divided into three types:
- Cataleptic, it is also called a disorder with waxy flexibility. The patient stops for a long time and freezes in a constant position, which can be completely uncomfortable for him. It is noteworthy that with complete non-reaction to human words spoken in a full voice, the patient may show a reaction to words spoken in a whisper. Sometimes the loosening of the bonds of stupor can occur at night.
- Negativistic stupor is characterized by the same symptoms as in the previous case, but the patient tries in every way to prevent the doctors from changing his position.
- Stupor with numbness is the most inhibited, with a strong motor stop, during which there is a significant increase in muscle tone. The patient is typically in the fetal position; the disorder may change to pathetic or impulsive agitation.
Catatonic agitation
This type of pathology also has several manifestations:
- The pathetic excited state gradually gains momentum, while the patient is distinguished by high spirits and cheerful behavior. After some time, excitement increases, pathetic and exalted phrases appear in speech, and echolalia slips through. In the final version, the pathology acquires a foolish mood, manifests itself in aimless behavior with complete preservation of consciousness, the patient can somersault and exhibit childish behavior. The patient is aware of his inappropriate behavior and is sincerely perplexed about what is happening to him.
- The impulsive form of excitement flares up suddenly, the main characteristic features are cruelty, speed and destruction of surrounding things and objects. Often there is aimless, repeated and persistent muttering or shouting of words and phrases, and the patient repeats some actions several times. A person crawls, spits, attacks someone, imitates the poses and actions of other people. In this condition, the patient can pose a significant danger to surrounding people or animals.
- Silent agitation is characterized by sudden, senseless aggression that is directed at other people. During such silent hatred, the patient causes severe injury and damage to himself and others, and violently resists. This behavior refers to the highest manifestation of impulse excitation.
Treatment of stuporous conditions
Treatment of stupor should be carried out in a hospital. In all cases, it is necessarily carried out against the background of therapy for the underlying disease.
If the diagnosis is unclear, additional examinations may be required to clarify it (EEG, computed tomography, laboratory tests, etc.)
This is also important in cases where there is a need to determine whether stupor is the result of somatic or mental illness
Treatment of the underlying disease should be quite intensive, taking into account the seriousness of the condition. At the same time, this is a prevention of relapses of stupor in the future. Of course, the range of drugs may be different: for example, antipsychotics if a patient has schizophrenia, anticonvulsants for epilepsy, antidepressants for depression, etc.
For functional pathologies (hysteria, stress, neuroses, etc.), psychotherapy can have a good effect.
Along with this, it is necessary to use drugs that disinhibit and stimulate the activity of the central nervous system. For these purposes, activating agents and psychostimulants (caffeine, Frenolone, Sidnocarb, etc.) are successfully used. As an additional therapy, the prescription of nootropic drugs (Piracetam, Encephabol, Phenotropil, etc.) can be considered appropriate.
In a psychiatric hospital, barbamyl-caffeine disinhibition is successfully used to treat many types of stupor (catatonic, depressive, etc.): intravenous administration of 1-2 ml of a 20% caffeine solution, and after 3-5 minutes 5-10 ml 5 % barbamyl solution. This method is also effective when patients refuse to eat.
For catatonic stupor, intramuscular administration of Frenolone at a dose of 5-15 mg per day is also used. For hallucinatory stupor, neuroleptics are used - Mazeptil, Triftazin, Haloperidol, etc. In the treatment of emotional, apathetic, hysterical stupor, tranquilizers - Diazepam, Phenazepam, etc. can be used.
In general, the specific choice of drugs and dosage are determined by the attending physician, based on the form of the disease and the severity of the patient’s condition.
Some of the possible complications of stupor have been mentioned above. In particular, emotional stupor can lead to the development of panic neurosis and depression.
Depressive, catatonic and epileptic forms of stupor can suddenly turn into a state of agitation with aggressive actions towards oneself and others. Stupor due to somatic diseases can be complicated by transition to stupor and coma.
Many of these conditions pose a threat not only to the health, but also to the life of the patient, and are also dangerous to others, which makes intensive treatment for stupor mandatory.
Emergency care for stupor
Emergency care for stupor comes down to preventing dangerous actions and ensuring the safety of the patient. With catatonic stupor, this is a readiness to stop sudden impulsive excitement. In case of depressive stupor - preventing the possibility of sudden development of depressive agitation with a desire for suicide, as well as eliminating refusal to eat. It should be borne in mind that psychogenic stupor can be replaced by psychogenic agitation. Emergency care for catatonic stupor in out-of-hospital conditions does not make sense, since attempts to disinhibit the patient can cause agitation and thereby create additional difficulties.
What are the symptoms of stupor?
A person who is in a stupor can be disturbed or awakened by vigorous stimulation. It may be considered unconscious, but may be partially responsive to stimuli. Stupor differs from coma in that a person in a coma cannot be awakened or stimulated at all.
Stupor may cause the following physical symptoms in addition to mental symptoms:
- abnormal breathing, where breathing is too slow or fast
- muscles are contracted in an abnormal way
- pupils that are wider or narrower than normal
- pupils that do not respond or change when exposed to light
There may be other disease-specific symptoms associated with stupor.
Stupor
Stupor
(from Latin stupor “numbness, stupor”) - in psychiatry, one of the types of movement disorder, which is complete immobility with mutism and weakened reactions to irritation, including pain. There are various types of stuporous states: catatonic, reactive, depressive stupor. Catatonic stupor is the most common; it develops as a manifestation of the catatonic syndrome and is characterized by passive negativism or waxy flexibility or (in the most severe form) severe muscle hypertension with numbness of the patient in a pose with bent limbs.
Being in a stupor, patients do not come into contact with others, do not react to current events, various inconveniences, noise, wet and dirty bed. They may not move if there is a fire, earthquake or some other extreme event. Patients usually lie in one position, the muscles are tense, the tension often begins with the masticatory muscles, then goes down to the neck, and later spreads to the back, arms and legs. In this state, there is no emotional or pupillary response to pain. Bumke's syndrome—dilation of the pupils in response to pain—is absent.
How to get out of a stupor
Only specialists—psychotherapists, psychologists, psychiatrists—know exactly how to overcome stupor. But if you see that a person close to you is in this state how to get out of the stupor, he definitely needs help, here are a few ways:
- Massaging special points that are located above the pupils of the eyes, exactly in the middle, equidistant from the eyebrows and the beginning of the hairline, can help; these points need to be massaged with the pads of the fingers, index and thumb;
- you can try to evoke any strong emotions in the patient, even negative ones - tell him something in a clear and confident voice, sometimes even a slap in the face helps;
- stupor can go away if you bend the person’s fingers and press them forcefully against the palms, the thumbs should remain straight.
Questions and answers
Question:
Good day. I am 21 years old. When I start communicating with someone, I feel some kind of stupor, I can’t say anything, I can’t carry on a conversation, there’s some kind of mess in my head. If I want to tell something, I often forget the words and get lost. I’m afraid to stay with a person one-on-one, I think that he will be bored with me. In the company of friends, all I do is listen, although when there is a conversation about something, I understand that I can tell a lot, express my opinion . Sometimes I think that I am inattentive and “dumb”. I myself am interested in psychology, football, technology, but when these topics are discussed, I am still afraid to say something. It feels like a cockroach is sitting in your head and doesn’t allow you to get used to the information and express yourself competently. The problem started back in school, when conflicts with classmates began, then the situation improved a little, but I became a boring person who is often silent, and when he wants to say something, he blurts out some nonsense, but only then do I realize it. Tell me what could be the problem?
Answer: The problem is the fear of other people’s assessment of their statements, actions, and deeds. Fears inhibit communication, and this “inhibition” makes one feel ashamed. Shame is an affective feeling; it practically paralyzes both the thinking and the active processes. Anger at oneself and lack of self-acceptance appear. Perhaps this is roughly what is happening to you. You might want to take individual or group classes to reduce your fears and discover that you are not the only one, many experience similar feelings. Then it will be easier to accept yourself and cope with your fears.
Question:
When the teacher asks something, I can’t say anything, because it’s like there’s some kind of stupor. I speak normally with my friends, no problem. It also happens that in a minibus I have to tell them to stop at the bus stop, but I can’t say a word, or in a store. How to deal with this?
Answer: It seems to me that the fear of speaking appears in you in situations where you do not feel that you are on an equal footing with the interlocutor (as happens with friends: you are on the same level with them). In frightening situations, there is a feeling that you should be evaluated (by the teacher or people on the minibus). Perhaps this fear of being assessed (most likely, a low assessment) is what causes stupor: it’s better not to say anything than to “blurt something stupid” and embarrass yourself. In such cases (if this is your case, of course) you can work with self-esteem, self-acceptance - non-judgmental. Maybe you are too hard on yourself? In addition, there are a lot of tricks that, for example, speakers use when speaking in front of a large audience. The fact is that the fear of public speaking is inherent in a huge number of people. To calm down before going out in public, speakers use different things: breathing (several deep breaths, exhalations, for example), visualization (imagine that you are among friends - just chatting carefree). There are special exercises to help improve diction, including for moments when your throat gets dry. You can combine the practice of such exercises and work to increase self-esteem and self-confidence.
Causes
The most common cause of catatonic syndrome is a mental disorder, but only a few of them can produce similar symptoms. The affective spectrum of pathomanifestations is quite extensive, but it is the catatonic syndrome that may be characteristic of mania, and this is not a typical form of mania, which requires a very detailed investigation and diagnosis. The classic catatonic syndrome is catatonic schizophrenia. With it, this disorder is most widespread and has a fairly typical course.
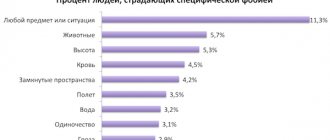
Severe forms of PTSD also have catatonic inclusions, but for them this is not a pathognomonic syndrome. Postpartum mental spectrum disorders can often reach the level of psychotic symptoms, including catatonic inclusions. Hysteria often imitates a large number of disorders that have very serious symptoms, and this pathology is no exception to the list of diseases, the symptoms of which are often used by the hysterical group of disorders. Autism is classified as part of the schizophrenia spectrum according to some sources, and it can also become the root cause of the described disease.
Catatonic syndrome in children is often provoked by autistic disorders. In children, it is provoked by all autism spectrum disorders. Various etiological disorders in children also become predictors of this syndrome. Neurological diseases are very close to mental disorders, which is why almost each of them can provoke this syndrome.
Tourette's syndrome, manifested by violent, uncontrolled screams, actions, and grimaces, can be accompanied by catatonic syndrome, as well as temporal lobe epilepsy, which even has an alter term - ictal catatonia. TBI and traumatic lesions leading to residual brain effects often provoke severe catatonic syndromes, especially with incorrect or absent treatment.
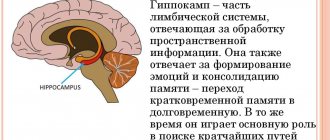
Cancerous lesions, especially those with a specific brain localization, very often provoke catatonic syndrome, and there are many oncological pathologies that provoke this symptomatology. Not only can the primary tumor be localized in the brain tissue, quite often a metastatic lesion becomes even more dangerous when it is carried into the brain tissue by the bloodstream. Depending on the proportion affected by these tumor tissues, a variety of productive symptoms may appear, including catatonic syndrome. Damage to the thalamus, postencephalic syndrome, is dangerous in this regard. Often, catatonic manifestations occur when the functioning of the globus pallidus, as well as the vertex and frontal part of the brain is disrupted.
Somatic pathologies also become very active predictors of catatonic syndrome, especially when the pathology is severe or even incurable. This happens with hematological pathologies, in particular platelet purpura. Severe disorders with metabolic disorders, such as endocrinopathies, with hyponatremia, Wilson's pathology, very often provoke this disease. Also, Tay Sachs disease and endocrinological disorders, either in the direction of hyperfunction or in the direction of hypofunction, may be involved in the development of pathology. As for thyroid pathology and adrenalism, such dysfunctions quite often manifest themselves as catatonic syndrome with severe decompensation.
Viral infections, especially AIDS, can cause this syndrome in the structure of brain damage. Also, hypovitaminosis B12 and typhoid infection are pathognomonic for this disorder. Autoimmune pathologies, especially those with damage to the blood vessels of the brain, are also predictors of this syndrome.
Paraneoplastic syndrome, as a manifestation of tumor-volitional pathology, various physical factors, such as lack of oxygen, heat constriction, poisoning with toxins and lead, often provokes catatonic syndrome. In addition, it can be caused by drug use, as well as antipsychotic drugs, antibiotics and some groups of anticonvulsants.
Symptoms of stuporous catatonia
Stuporous catatonia is characterized by immobility during which people may assume rigid positions (stupor), an inability to speak (mutism), and a waxy flexibility in which they maintain positions after someone has placed them in them. Mutism may be partial, and they may repeat meaningless phrases or speak only to repeat what someone else says. People with dull catatonia may also exhibit stereotypic, repetitive movements (stereotypy). Excited catatonia is characterized by strange, non-goal-directedness and impulsivity.
Catatonia is a syndrome that can occur in a variety of mental disorders, including major depressive disorder, bipolar disorder, schizophrenia, schizoaffective disorder, schizophreniform disorder, brief psychotic disorder, and substance-induced psychotic disorder. It manifests itself as Kahlbaum's syndrome (immobile catatonia), malignant catatonia (neuroleptic malignant syndrome, toxic serotonin syndrome) and excited forms (delusional mania, catatonic agitation, oneirophrenia). He has also been assessed for autism spectrum disorder.