The mental health of each person is a very delicate matter, the slightest fluctuations of which can lead to a number of negative consequences for the subsequent full-fledged social life.
In the modern world, according to statistics, every fifth resident of a large city is a carrier of a certain type of mental disorder. This is caused by an overactive rhythm of life, chronic fatigue and frequent stressful situations. The danger is that some people may not be aware of their illness for many years, attributing everything to fatigue and workload. And only at the moment when a failure occurs, it becomes clear that the reasons lie much deeper and it is necessary to look for them with a qualified specialist. Treatment of mental disorders. Symptoms and signs
Today, medicine knows many mental illnesses, which differ in different types of manifestation. However, there is one connecting link between all disorders - this is a combination of abnormal thoughts, emotions and behavioral reactions aimed at the patient himself or at people around him.
The most common mental health disorders are:
- depression;
- schizophrenia;
- panic attacks;
- eating disorders (anorexia, bulimia);
- mental retardation;
- autism;
- bipolar affective disorder;
- psychoses.
The specialized clinic “Salvation” provides a wide range of services and high-quality treatment for mental disorders. The symptoms and signs of each individual disease have their own character, which is why a competent approach and properly selected support guarantee significant improvements in health in the shortest possible time. Therefore, if you find that the behavior of your relatives has changed, they forget the names of objects, dates, faces, you should not self-medicate. Such signs indicate mental disorders and require the experienced eye of a specialist.
Symptoms of mental disorder
Each mental illness begins with the appearance of various symptoms, which, as a rule, one at a time do not raise any special questions from others and it can be difficult to collect them all into a single picture. However, careful observation of a person over several days will allow us to draw conclusions for taking further measures.
Symptoms of mental disorders in most cases are closely related to a person’s depressed state, which prevents him from performing daily routine activities. These symptoms include:
- physical (sleep disturbance, both in the direction of insomnia and vice versa, constant loss of strength even after proper rest; headache, etc.);
- behavioral (abuse of pills, cigarettes and other substances in large quantities, inability to perform work);
- cognitive (inability to think clearly, memory problems);
- perceptual (obsessive thoughts);
- emotional (constant feelings of anxiety and sadness).
The presence of several symptoms immediately indicates a problem and the need for professional consultation with a psychologist or psychotherapist. Identifying the causes and the possibility of making a diagnosis in the early stages will help quickly get a person out of such an undesirable state.
Generalized anxiety disorder
- How common: 284 million people worldwide experience symptoms of anxiety disorders.
We all experience anxiety from time to time, but usually the anxiety goes away Generalized anxiety disorder as soon as the stressful situation ends. But people with generalized anxiety disorder do not. Fear and anxiety are constantly present in their lives, making it difficult to carry out daily activities. At the same time, they do not always need a specific reason for their experiences. Things may be going well, but a person will still look for reasons to worry. For example, thinking through negative scenarios for your actions or worrying that something bad could happen to your loved ones at any moment.
The diagnosis is made if Generalized anxiety disorder similar symptoms persist for six months:
- strong feelings that clearly exceed the seriousness of the situation;
- long thinking about minor events, constant assessment of possible unsuccessful outcomes;
- fear of making decisions due to the risk of making mistakes;
- inability to relax and let go of the situation;
- a permanent state of being “on edge” - when every little thing can make you angry;
- sleep problems;
- pain in the head or stomach in the absence of physical illness;
- nausea, diarrhea, need to go to the toilet more often.
Causes of mental disorders
Some deviations in mental health can be caused by absolutely understandable reasons, for example, damage to a certain area or the entire area of the brain, traumatic brain injury, intoxication or problems with blood vessels. While depression, schizophrenia and a number of other diseases are not tied to a specific factor, and even with numerous studies, it has still not been possible to establish an unambiguous cause for the development of pathologies.
The causes of mental disorders are:
- internal (genetics; developmental disorders at a certain stage of pregnancy; developmental abnormalities at an early age; somatic diseases that affect the functioning of the brain; immunological disorders; hormonal imbalance, etc.);
- external (chronic stress; alcohol and drug intoxication; consequences of encephalitis or meningitis infections; traumatic brain injuries; exposure to radiation).
Most often, the causes of mental disorders are a combination of various factors when, for example, an organism weakened by infections finds itself in a highly stressful environment. The presence of each factor and its level of effect on a particular person must be assessed by an experienced specialist.
Most doctors approach mental health disorders as a multifactorial disease, since even if the main cause of the problem is known, related issues also play an important role and must be taken into account in the treatment process. These include:
- human living conditions;
- features of upbringing and traditions in the family;
- surrounding society;
- general health;
- work and family environment;
- originality.
What happens in the body during mental disorders?
Some psychiatrists believe that about a quarter of the world's population will develop some form of mental disorder at some point in their lives. From my point of view, this is clearly an underestimate, since depression and anxiety, personality disorders and substance abuse, post-traumatic stress disorder and various phobias are, of course, much more common. On the other hand, our patients more often turn to psychologists, ministers of various religious cults, psychics, and healers than to psychiatrists. Usually, the patient comes to the psychiatrist last, and then usually at the insistence of his relatives. In my opinion, a psychiatrist should really be the last resort, since most so-called mental disorders can be treated by neurologists and psychotherapists, not to mention the specifics of narcologists and sexologists. This is not even the point, a huge number of mental disorders arise secondary, due to damage to various organs, including organic damage to the brain, whether it is caused by infection, intoxication, trauma, tumor or some clearly autoimmune process. And it’s funny to think that these reasons have disappeared somewhere or that the mechanisms of pathogenesis have become somehow different.
I am convinced that in the near future we will use psychotropic drugs less and less, since the latter do not relate to the causes and mechanisms of the formation of mental disorders. You may ask, how will we treat a patient suffering from a mental disorder? I will answer: immunotopic and neurotropic, hormonal and metabotropic, antimicrobial and cardiovascular drugs, etc. And, this is a huge arsenal of drugs! However, we have long been doing in our clinic assigning psychotropic drugs an auxiliary, and not the main role in the treatment of mental disorders.
However, in this note I would like to say a few words about metabolic disorders that occur in mental disorders, including those metabolic disorders that occur both in the structures of the brain and in other organs and systems of the body. To approach this problem, it is important for us to answer the question of what happens in the body during mental disorders (put in the title of my note), and if we find out, we will probably try to eliminate these metabolic syndromes, which will undoubtedly contribute to the recovery of our patients .
So, it is reasonable to assume that disturbances in the energy metabolism of brain cells accompanies any mental disorder; of course, this disorder can be expressed differently, have certain specifics and, therefore, its own methods of correction. It is interesting to note that studies in schizophrenia identified 92 differentially expressed proteins associated with energy metabolism, while 95 proteins were found in bipolar affective disorder and 41 proteins in major depressive disorder.
Unfortunately, only a small minority of psychiatrists believe that all of these mental disorders are caused by small defects in a few areas of the brain, rather than by large damage in a single area of the brain. This implies that these disorders may occur due to defective connections between brain structures.
It is known that our brain makes up only 2% of the total body weight and, paradoxically, is responsible for ~ 25% of the total glucose consumption in the body. Glucose is an essential energy substrate of the brain, and it flows through many reactions to produce adenosine triphosphate (ATP) through sequential processing by glycolysis, the tricarboxylic acid (TCA) cycle, and oxidative phosphorylation (OXPHOS). Oxidative metabolism is a key process in maintaining cell viability as it generates large amounts of ATP, however this accelerated rate of oxidation in the cell results in the formation of potentially harmful byproducts called reactive oxygen species (ROS). These elevated levels of ROS, if not neutralized by the action of antioxidant enzymes, can cause disturbances in the metabolism of carbohydrates, lipids, and proteins, which can lead to functional deficits and even death of brain cells. Consequently, antioxidants are able to protect our brain from a pathological process that is externally manifested by disturbances in thinking, emotions and behavior.
Glucose also plays an important role in the metabolic processes (biologists speak in "pathways") that lead to the synthesis of glutamate, acetylcholine, and gamma-aminobutyric acid (GABA), all three of which are key neurotransmitters in the central nervous system. Mitochondria, which play an important role in cellular energy production, also help buffer calcium and neutralize reactive oxygen species and are closely linked to amino acid metabolism.
The brain's high energy demand is driven primarily by a variety of energy-intensive processes, including axonal action potentials, cell signaling, presynaptic Ca2+ entry, neurotransmitter uptake and recycling, and synaptic vesicle release (exocytosis). Gray matter regions of the brain contain a majority of excitatory synapses relative to inhibitory synapses, suggesting that excitatory neurotransmission accounts for the majority of energy demands at the cortical level. Depending on the activity(s) performed by us at that time, the energy consumption in the corresponding area of the brain is stimulated and for this reason, there is an increase in blood flow to that particular area as the energy substrates reach their targets through the circulatory system, which can be monitored by functional magnetic resonance imaging or a simpler version of near-infrared spectroscopy.
Analysis of blood samples from patients with schizophrenia revealed elevated insulin levels and increased insulin resistance. From the history of psychiatry, we know about an almost forgotten method of treating schizophrenia using insulin shock therapy. So, what is it that we don’t understand: is insulin our friend or enemy when it comes to a mental disorder, in particular schizophrenia? In addition, we also know, again from the relatively recent history of psychiatry, that depression-resistant patients or patients suffering from eating disorders have also been treated with small doses of insulin. The thought arises: maybe in all these cases we have pathogenetic treatment aimed at correcting carbohydrate metabolism in brain tissue. True, we did all this blindly and often with serious side effects; however, psychotropic drugs, as we know, are also not angels and can lead to both insulin resistance in metabolic syndrome and diabetes mellitus.
In schizophrenia, a higher prevalence of hyperglycemia (most likely in the acute phase of psychosis, accompanied by psychomotor agitation) and impaired glucose tolerance was also revealed compared with healthy people. Many researchers have found a correlation between the occurrence of psychosis and changes in blood flow and metabolism in various areas of the brain.
Patients with untreated schizophrenia were studied using 18 F-fluorodeoxyglucose positron emission tomography (PET) and magnetic resonance imaging (MRI) to assess glucose metabolism and obtain volumetric measurements, respectively. This study found that, compared with controls, patients with schizophrenia showed lower relative rates of glucose metabolism and volumetric contractions of brain cells in the cingulate cortex, precisely those thought to be associated with higher executive functions (planning, forecasting, problem solving, etc.) .). In a similar study that focused on the three nuclei of the thalamus, it was noted that a decrease in relative glucose metabolism in the pulvinar nucleus was associated with more hallucinations and other so-called “positive symptoms” (delusions, thought disorganization), while “metabolic contractions of brain matter” in the mediodorsal nucleus were associated primarily with negative symptoms (apathy, alogia, affective flatness, anhedonia, abulia). There have also been reports of significantly lower pyruvate levels in the mediodorsal thalamus in patients with schizophrenia.
Schizophrenia is also associated with mitochondrial dysfunction and the presence of mutations and polymorphisms in mitochondria. Mitochondrial hypoplasia has also been observed in addition to significant changes in the enzymatic activity of Complex I, located in the inner mitochondrial membrane, which together indicate dysfunction of the oxidative phosphorylation system and decreased ATP production in patients with schizophrenia. Impairments associated with oxidative stress are evident in schizophrenia, manifested by higher levels of superoxide dismutase (SOD) and glutathione peroxidase (GSH-Px) activity. Another important cellular process associated with mitochondria is the maintenance of calcium homeostasis, and studies have shown disruption of calcium homeostasis and signaling in schizophrenia. All of these metabolic processes altered in schizophrenia are involved in synaptic remodeling, and their dysfunction can cause a wide range of deleterious effects and therefore affect the brain's plasticity and ability to recover from mental illness.
Several factors associated with metabolic syndrome, including obesity, diabetes, and hyperglycemia, are associated with the presence of depression; and there are reports of insulin resistance in patients with major depression. Positron emission tomography measurements in patients with major depressive disorder revealed a decrease in both blood flow and glucose metabolism in the caudate nucleus, anterior cingulate cortex, and prefrontal cortex during tests that were performed both at rest and in stressful situations. However, analysis of the orbital cortex, medial thalamus and amygdala showed an increase in blood flow and glucose metabolism. Another study used stable isotope injection (13C) magnetic resonance spectroscopy (MRS) to evaluate processes associated with neurotransmission and metabolism in patients with major depressive disorder. It could be observed that glutamatergic neurons showed impaired TCA cycle rates compared to controls, which meant that the glutamatergic system and mitochondrial energy metabolism may play an important role in the pathogenesis of this mental disorder. Consistent with these findings, patients with major depression showed significantly impaired mitochondrial ATP production and lower levels of mitochondrial enzyme activity compared with controls. In addition, a large proportion of patients had deletions in mitochondrial DNA (mtDNA), which also indicates the presence of mitochondrial dysfunction.
Patients with bipolar disorder have a higher incidence of metabolic syndrome compared to the general population. While collecting data on the prevalence of metabolic syndrome, we noted that the frequency of metabolic syndrome varied from 17 to 67% in patients with bipolar affective disorder (manic-depressive psychosis). Research has shown that people with bipolar disorder are more susceptible to hyperglycemia, type 2 diabetes, and insulin resistance than the general population. Monitoring cerebral blood flow in people experiencing symptoms of mania showed that, compared to healthy controls, there was a decrease in blood flow in various areas of the brain, particularly the right ventral region and frontal region. Interestingly, another study confirmed that manic patients had higher cerebral blood flow in the anterior cingulate cortex of the left hemisphere of the brain.
Evaluation of markers commonly associated with metabolic dysfunctions revealed lower serum levels of glucagon, glucagon-like peptide-1 (GLP-1), ghrelin and higher levels of glucose-dependent insulinotropic polypeptide (GIP) in patients with bipolar affective disorder. Glucagon is known to act on the psychological stress response system. It is worth noting that GLP-1 and GIP receptors are expressed in brain regions predominantly involved in mood regulation and cognitive functioning. Therefore, these markers may be critical to the relationship between bipolar and metabolic disorders as they serve important roles in the mechanisms of brain synaptic plasticity and neuroprotection, which have been found to be altered in neuroimaging studies of patients with bipolar disorder Gray matter analysis in patients with bipolar disorder without medication revealed increased lactate levels and decreased intracellular pH in the prefrontal cortex. These characteristics suggest that cells rely primarily on glycolysis rather than OXPHOS for energy, which in turn may indicate that mitochondrial functionality is impaired in this mental disorder.
The goal of proteomics is to gain a general understanding of the proteins present in a given cell or tissue at a particular time and in a particular state; only this "snapshot" is possible because the proteome is dynamic and changeable, with different proteins constantly being degraded and produced in response to various internal and external stimuli. The proteome represents the genetic information that has been transcribed and translated after any modifications at the epigenetic, mRNA and post-translational levels. Based on the above, it has been suggested that proteomics may provide more accurate information about the pathogenesis of disease and mental disorder in particular than other approaches such as genomics and transcriptomics, since it represents which proteins are present at any important point during the course of a disease. Thus, mass spectrometry (MS)-based proteomics techniques have been widely used in several studies due to their ability to identify as well as quantify multiple disease-associated protein changes in a given tissue sample.
Proteomic methods used in the study of neuropsychiatric disorders began with the development of two-dimensional gel electrophoresis (2DE). By the end of the 1990s, two-dimensional differential electrophoresis (2D-DIGE) had already been developed. The main limitation of 2DE and 2D-DIGE methods is the separation of proteins with more extreme characteristics, including those that are hydrophobic, too big or too small, or extremely basic or acidic. Despite their limitations, these methods provide a high-quality, top-down approach to complete proteome resolution, protein isoform resolution, and post-translational modifications. In 1999, a protein identification technique was described using first liquid chromatography (LC) and then tandem mass spectrometry (MS/MS) to separate and fragment peptides. Based on this, the term “shotgun proteomics” was coined. This approach is continually being refined to provide better coverage of the entire proteome. Modern proteomic studies consist of digested proteome analysis that undergoes chromatographic separation of one or more dimensions followed by MS/MS analysis.
Proteome analysis in schizophrenia, bipolar affective disorder and major depressive disorder showed that five proteins overlap: aldolase C, citrate synthase, malate dehydrogenase, cytochrome bc1 core protein 1 and ATP synthase beta subunit. Thus, we see new targets for the treatment of these mental disorders. Let's take a closer look at these squirrels. Aldolase C is an essential enzyme in glycolysis, responsible for the conversion of fructose-1,6-bisphosphate to glyceraldehyde-3-phosphate and dihydroxyacetone phosphate. Citrate synthase is a key enzyme in the TCA cycle and catalyzes the reaction in which citrate is formed by the condensation of the acetate moiety from acetyl-CoA with oxaloacetate. Malate dehydrogenase is another enzyme of the TCA cycle and catalyzes the NAD+/NADH-dependent interconversion of the substrates malate and oxaloacetate. Cytochrome bc1 core protein 1 is found in the mitochondrial matrix, and the complete cytochrome bc1 complex is a key component of the respiratory electron transport chain embedded in the inner mitochondrial membrane. The beta subunit of ATP synthase is the part that is responsible for converting ADP to ATP, which occurs due to the proton gradient across the membrane formed by OXPHOS reactions. These differences relate to the major axis of ATP production metabolic pathways, with little emphasis on oxidative phosphorylation. The overall differential expression of citrate synthase and malate dehydrogenase could hypothetically link these abnormalities to impaired lipid production. Citrate synthase is downregulated in schizophrenia and elevated in bipolar disorder and major depressive disorder, whereas malate dehydrogenase is downregulated in bipolar disorder and elevated in schizophrenia and major depressive disorder. This disruption in ATP production can switch the cell's metabolic demand for energy through the breakdown of lipids in the brain.
Phospholipase A2 (PLA2), which catalyzes the breakdown of membrane phospholipids, has been found to have increased levels of activity in the blood of patients with schizophrenia. There have been reports of increased phospholipid turnover rates in the thalamus and frontal lobe and lower levels of docosapentaenoic acid (EPA) and phosphatidylcholine in the hippocampus of patients with schizophrenia. In addition, there is evidence of lower levels of arachidonic acid (AA) in the red blood cells and brain tissue of patients with schizophrenia. Increased rates of hydrolysis of serum phospholipids in bipolar disorder and increased levels of prostaglandins—compounds derived from AA metabolism—have been reported in the serum, saliva, and cerebrospinal fluid of patients with bipolar disorder. Upregulation of calcium-dependent cytosolic phospholipase A2 (cPLA2), an enzyme involved in AA metabolism, as well as lower AA concentrations in the frontal cortex of patients with bipolar disorder have also been reported.
Cholesterol, located in the myelin sheath that surrounds axons, is effectively immobilized due to the slow turnover of myelin. Studies conducted on patients with mood disorders have shown lower cholesterol levels compared to controls. There was a significant association between the ratios of AA and EPA present in red blood cells and the severity of depression. Compared to healthy controls, patients suffering from major depressive disorder were found to have significantly higher serum levels of PLA2 activity, and PLA2 mRNA expression was significantly increased compared to healthy controls. Several studies have shown the effects of antidepressants, antipsychotics, and mood stabilizers on PLA2 activity. The antipsychotic drug clozapine has been reported to increase red blood cell AA and docosahexaenoic acid (DHA) levels in patients with schizophrenia. This may indicate an additional mechanism that contributes to the therapeutic effects of clozapine. Lithium at therapeutic concentrations has also been shown to potently inhibit PLA2 activity.
. In fact, major depression has been described as an initial symptom of mitochondrial disease in a large sample size of adult patients. Mitochondrial function and energy metabolism have been shown to play important roles in regulating social behavior. Data from many studies show that schizophrenia and bipolar disorder share 32 altered proteins. We emphasize that these two disorders have similar chronic and recurrent disease trajectories. Changes in electron transport chain components, such as subunits of NADH dehydrogenase or glycolytic enzymes such as pyruvate kinase and phosphofructokinase, reveal a general dysregulation of energy metabolism that may be associated with dysfunctions in mitochondrial processes.
(Figure 1
Signs of mental disorder
The peculiarity of mental illness is that there are no conditions, ages, nationalities or races for them. Absolutely every person, especially in the current world of multitasking and constant stress, is susceptible to threat. You can recognize the signs of a mental disorder with some careful observation of the behavior of others and your own.
- No matter how crazy you go. Everyone has fear - of newness, forgetfulness, a pressing deadline, natural disasters and other similar things. Constant thoughts around what a person is afraid of, together with a series of nervous situations at home or at work, can cause neurosis and panic attacks. And when mental health is shaky, psychosomatics can also get involved. In such a set it is difficult to find the root cause, and the neglected process can result in a more serious mental illness.
- Absent-mindedness. Conditions of constantly tight deadlines have a strong impact on the nervous system. It’s simply physically impossible to do everything, and you become distracted and forgetful. The nervous system cannot cope with overstrain and fails. As a result, the development of a mental disorder.
- Not good enough. Beauty standards, fashion canons, and high standards lead to the emergence of a whole complex of mental illnesses. This includes depression, eating disorders and psychosis. N
- Addiction. In addition to addiction to various alcoholic and psychotropic substances, which cause many mental disorders, psychologists have found that workaholism can also lead to unwanted diseases. Constant immersion in work matters, sleep disturbances and emotional burnout are slowly and surely preparing another person who needs the help of a psychotherapist.
People with mental disorders
As already mentioned, every person is susceptible to mental illness to varying degrees. Unfortunately, a healthy lifestyle and careful treatment of the nervous system cannot always guarantee the effect of “vaccination” against such diseases. People with mental disorders are not always the ones you often see in films. Not everyone wears white straitjackets, hears voices and sees things that others don't. Most people suffering from mental disorders are ordinary passersby whom you can meet on the way to work, neighbors at the nearest table in a coffee shop, and even friends and family. However, there are also more serious forms of the disease.
Prognosis of the course of personality disorder
Most people who receive treatment recover from their personality disorder over time.
Psychotherapeutic or medical treatments provide significant relief and can often be recommended even for people with mild personality disorders as a form of support. This depends on the severity of the disease, and on the presence of other ongoing problems. Some people with mild to moderate personality disorder benefit from specific psychotherapy, which is very helpful.
However, there is no single approach or any unified psychotherapeutic techniques that could suit everyone, so treatment must be selected taking into account the individual characteristics of personality development. It is very important that therapy for personality disorders is carried out by a qualified psychotherapist.
Mental disorders in adults
Most mental health problems in adults arise and develop against the general background of dissatisfaction with life, as well as particular stressful situations that can be accompanied both in the family and at work.
Bipolar disorder has gained widespread popularity because the number of patients it reaches is frightening. The disease manifests itself through frequent uneven mood swings, when a person, from vigorous activity, is transferred to a period of complete powerlessness, with the inability to eat, move and continue a full life.
Another most common mental disorder in adults is depression. Despite the fact that psychologists have long been trumpeting the danger of this disease, modern society still does not pay due attention to it and subsequently specialists have to treat more advanced forms that the person himself is not able to cope with.
Schizophrenia. May arise from dissociative identity disorder or as a separate disorder. As a rule, the disease develops against a background of disharmony and a tense nervous state over a long period of time, but schizophrenia can also develop on a completely stable neurological basis.
Women, as a separate category, are more susceptible to mental disorders than men. The most common diseases include manic-depressive psychosis, eating and sexual behavior disorders, delirium and alcohol addiction, nervousness and panic attacks.
Depression
- How common: every sixth person experiences What Is Depression? with depression at least once in your life.
The trigger for the occurrence of this disorder is various situations: loss of a job, death of a loved one, illness, childbirth.
The main symptom of Clinical depression is depressed mood. But unlike sadness, depression cannot be overcome by “just getting a grip.” In this state, favorite activities such as communication with loved ones, sports, sex do not bring pleasure. Therefore, gradually a person loses interest in them. Many people's self-esteem drops and it becomes difficult for them to make even the simplest decisions. And this exacerbates the feeling of worthlessness and helplessness. It becomes so difficult to bear these feelings that sometimes depression turns into thoughts of suicide or a desire to harm oneself.
Psychological symptoms may be accompanied by physical ones:
- loss of appetite or, conversely, excess in eating;
- constipation;
- unexplained body pain;
- weakness;
- menstrual irregularities;
- insomnia or constant sleepiness.
You should consult a doctor when these symptoms persist for more than two weeks. But if thoughts of suicide arise, help should be sought as quickly as possible.
During a period of depression, it may seem that no one is able to pull a person out of this state. But that's not true. With proper treatment, most people make a full recovery from clinical depression. At the EMC Psychiatry and Psychotherapy Clinic, experienced doctors work with depression of any severity and other mental disorders. Here they will help you correctly diagnose the disease and create an individual treatment program. When the disorder is severe, acute periods can be spent in an inpatient clinic. EMC provides support to the entire patient's family: there are programs that will teach you how to communicate with those who have mental problems and identify deterioration in time.
To learn more
Mental disorders in children
As every child goes through certain stages of his life, he faces a lot of problems and challenges. Some people endure all the difficult periods, but there are also those who are not ready for such conditions. Mental disorders in children can begin under the pressure of various factors.
- The formation process is often accompanied by the child’s rejection of himself and his own body. This causes various behavioral reactions, such as overeating or, conversely, refusing to eat. This eating disorder can lead to anorexia or bulimia.
- Peer bullying. Once one person stands out, he becomes a target for others. School bullying causes nervousness, psychosis, and depression. Suicidal thoughts may appear.
- Tense situation in the family. A very common cause of mental disorders in children is an unhealthy environment. If constant violence occurs in front of a child, then a mental disorder is guaranteed and can subsequently cause the development of schizophrenia. In an attempt to escape from reality, children invent a different life for themselves and stop this process, especially in an advanced stage. It can be extremely difficult.
- Congenital mental disorders of children can be caused by genetic predisposition, as well as unacceptable behavior of parents at the time of bearing the baby.
Levels of mental impairment
When diagnosing mental health diseases, doctors identify levels of mental disorder, depending on which decisions are made on further treatment and stabilization.
The first level is neurotic, which represents the appearance of various phobias, fears and neuroses, which can be caused by illness or some external factors. Divided into several types:
- neurasthenia (this implies nervous exhaustion of the body, weakness, apathy and irritability);
- obsessive-compulsive disorder (accompanied by an obsessive state when a person thinks that he hears or sees something that is not actually there);
- hysterical neurosis (refers to conditionally desirable types of disorder and begins when a person may benefit from it, although he himself may not be aware of such a reaction of the body).
The first level of violations is characterized by the beginning and end of the process in approximately limited periods. Such disorders most often affect people who have such a predisposition. However, various mental traumas can also trigger neurosis.
The second level is called psychopathic and is a reflection of all human personality disorders. These are certain nuances in behavior, as well as character traits that are present with a person throughout his life.
And the last level of disorders is psychosis (psychotic). This stage of the disease is accompanied by the appearance of hallucinations and delusions. Various manias, catatonia and mental confusion may also occur.
Types of Personality Disorders
Personality disorder is a group of mental disorders. They involve long-term, persistent changes in thought processes and behavior that are unhealthy and inflexible. There are several different types of personality disorders. The disorders can be grouped into one of three groups - A, B or C - which are listed below.
Cluster A personality disorders
A person with Cluster A personality disorder tends to have difficulty interacting with other people and would normally be considered strange and eccentric by most people. They can be described as living in a fantasy world of their own illusions.
An example is paranoid personality disorder, when a person, against the background of “exemplary behavior,” becomes extremely distrustful and suspicious.
Cluster B personality disorder
A person with Cluster B personality disorder struggles to regulate their feelings and often fluctuates between the positive and negative opinions of others. This can lead to patterns of behavior that can be described as dramatic, unpredictable and disturbing.
A prime example is borderline personality disorder, where a person is emotionally unstable, has impulses to harm himself, and has intense, unstable relationships with others.
Cluster C personality disorder
A person with Cluster C personality disorder struggles with persistent and overwhelming feelings of anxiety and fear. Such people can rarely show patterns of behavior; most people with this class will have antisocial and withdrawn behavior.
An example is avoidant personality disorder, where a person is painfully shy, feels socially inhibited, inadequate, and is extremely sensitive. A person may and often wants to be a good family man, but lacks the confidence to form close relationships.
Treatment of mental disorders
Depending on what disorder the patient suffers from, completely different treatment methods may be needed. In addition, it is worth considering that the treatment of mental disorders in each individual case is deeply individual and requires a careful approach.
The early stages of most diseases are not accompanied by severe problems, so doctors do not recommend placement in clinics and the use of aggressive therapy. If a person is independently able to recognize the presence of a problem, then the treatment process is based on consultations with a psychologist and psychotherapist and work to identify the causes that gave rise to the disease.
Diagnosing mental disorders in a mild form allows you to get by with “little blood” and build recovery in such a way that the patient will recover in a short time and can easily restore his mental health.
Treatment of mental disorders in adults
Mental disorders for different age categories differ in many ways, so the right approach to recovery is also selected taking into account the differences. For example, treatment of mental disorders in adults is often accompanied by the use of a group of antidepressant drugs, which is completely unacceptable when treating children.
Each disorder, be it autism or initial neurosis, requires its own techniques.
- Depression. Treatment methods should be selected based on the severity of the disease. Depression in the early stages can be cured using traditional methods, as well as through the processes of socialization, the introduction of an active lifestyle and periodic visits to a psychologist. If we talk about advanced cases, treatment includes constant observation by a psychotherapist, in-depth study of the causes of occurrence with a psychologist, hypnosis and drug intervention.
- In the first stages of development, doctors suggest treating bipolar disorder by restoring sleep patterns and giving up all substances that have a psychotropic effect on the human body (alcohol, drugs, tobacco). There are also effective medications that help prevent relapses. They are designed to stabilize the mood, protecting a person from depressing thoughts. Psychosocial support plays an important role in the treatment of bipolar affective disorder.
- Dementia is one of those types of mental illnesses that cannot be completely cured. Today, there are a large number of medications that are only undergoing clinical trials. Treatment methods for this disorder come down to an integrated approach and careful care of the person.
- Schizophrenia and neuroses in modern medicine can also be treated with medications, regular visits to psychologists and human socialization programs. Thanks to the correct management of the healing process, people suffering from this type of disorder can lead a full, happy life.
Treatment for Personality Disorder
Personality disorders are almost always associated with some organic changes in the central nervous system, so examination and observation by a neurologist is always necessary in such cases, and if it is not only a neurologist, but also a doctor of rehabilitation medicine, it will be much better!
The treatment process for a personality disorder is individual and often very lengthy.
Usually they take as a basis the typology of the disease, its diagnosis, the possibilities of introspection, habits, behavior, and response to a particular situation.
The additional clinical picture, personal psychology, and the patient’s desire to contact the doctor are also important. The latter is usually difficult with patients with dissatisfied personalities.
The results show that psychotherapy is very helpful for patients with personality disorder. The patient must be shown to a teacher (psychologist) and influenced by the social-environmental method. Thanks to such influences, it is possible to achieve harmony in the patient’s behavior and stabilize his behavior.
Recently, a new method has been used to correct the treatment of personality disorders with the help of psychopharmacological drugs. However, they will not solve the problem completely, since the task only introduces limitations with a corrective effect on psychopathological formations and phenomena. Therefore, treatment in a hospital is only “starting”, supporting in nature.
If treatment is started on time and correctly, the patient can be brought to a normal standard of living and practically cured.
Drug treatment for personality disorder
To dull feelings of anxiety, depression, and many other symptoms, you can use drug therapy. Patients use drugs such as SSRIs for depression and agitation. And anticonvulsant medications reduce excitability and anger. Some drugs like risperidone are prescribed to patients suffering from depression, an early stage of personality disorder.
Psychotherapy for personality disorder
People receiving treatment for personality disorders are generally unaware that they do have problems in their lives. They find it in other people, in society. Therefore, close people feel completely uncomfortable. Only a quarter percent of such patients intend to be treated, that is, they are aware of what is happening and turn to psychiatrists.
Treatment for personality disorder includes various forms of psychotherapy. Sometimes you have to resort to the use of pharmacological drugs.
A psychotherapeutic technique that is used both in individual and group sessions is successful in this regard. If necessary, this form of treatment can take place in couples and family settings. Taking into account all kinds of techniques and the set goal desired to be achieved during psychotherapeutic influences, the majority of psychotherapists note that the most difficult, but also very responsible aspect of treatment is to bring the patient into trusting contact. This is necessary in order to understand human problems and their internal sources.
Treatment of mental disorders in children
Most mental disorders in children are caused by adolescence and the stage of personality development. If symptoms indicating the development of deviations are detected, it is necessary to stabilize the atmosphere in the family as much as possible, spend more time with the child, talk about topics that concern him and support him in the first uncertain steps without criticism and intimidation. A visit to a psychologist and obtaining an expert point of view will also not be superfluous and will help you correctly plan the process of dealing with an unwanted illness.
Some diseases, such as schizophrenia, which appear already in adolescence, require mandatory drug intervention. However, many other disorders do not require the addition of medications to the treatment of mental disorders in children, therefore, the creation of harmonious relationships with oneself and society should be taken into the hands of parents or psychological professionals.
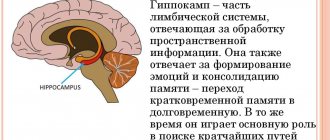
Organic mental disorders
Mental illnesses that occur when a particular area or entire area of the brain is damaged, due to various factors, are called organic mental disorders. This type of disorder includes multiple diseases that can occur due to external influences on the brain (traumatic brain injury) or internal processes (dysfunction). The main syndrome of organic disorders is damage to short-term memory. In such cases, a person remembers only those events, emotions and information that just happened. When repeated attempts are made to remember what happened, even after a few minutes, complete amnesia sets in. Often people “remember” certain moments in their lives, but when checked, this information turns out to be fictitious. The process of treating organic mental disorders includes an integrated approach, which involves medications, work with relatives and caregivers, as well as psychotherapy and psychopharmacotherapy.