Literally, the word “schizophrenia” is translated from Greek as “splitting / splitting of the mind / thinking.” With this disease, a person loses the ability to adequately perceive himself and the surrounding reality. This pathology has many forms and types. Each of them has its own symptoms. Impaired thinking in schizophrenia is observed in almost all cases. In this article we will consider the main aspects of this problem.
In this article
- Key Features
- What is thinking
- Operational aspect
- Motivational aspect
- Cognitive sphere in schizophrenia
Key Features
Most people believe that schizophrenia is a split personality disorder. However, this is too simple a definition. In fact, it is a more complex mental pathology that covers many different disorders. Most of them have nothing to do with the formation of new personalities in a person’s head.
According to ICD-10, a diagnosis of schizophrenia (F20.0-F20.3) can be made if at least one of the following symptoms is observed:
- Putting/taking away thoughts, their openness to others, “echo” of thinking. It seems to a person that strangers hear his thought process (or other people influence him by planting ideas or replacing memories).
- Crazy ideas. First of all, schizophrenics are concerned about delusions of influence. They are sure that their body or thoughts are influenced by surrounding or otherworldly forces, for example, aliens.
- Hallucinations - auditory, visual and tactile. Patients hear, see and touch what is not in reality.
- Persistent delusions. They are associated with culture, politics, invention, etc. As a rule, such nonsense sounds ridiculous or even fantastic.
A person may also be diagnosed with schizophrenia if two of the following signs are present:
- Persistent hallucinations of any type, accompanied by delusions, which appear over the course of a month.
- Sperrungs and neologisms are breaks in thinking, the use of non-existent words in speech.
- Catatonic syndrome - psychomotor (motor) disorders. The patient is either highly excited or falls into a stupor, freezing in an unnatural position for several hours.
- Negative symptoms: apathy, poverty of speech, lack of initiative, loss of interests, inadequacy of emotions, alienation, etc.
The last group of symptoms, negative, can also be observed in depression. However, in the presence of hallucinations, sperrungs or catatonic syndrome, which develop against the background of apathy and other signs of a negative type, the question arises of making a diagnosis of schizophrenia.
Thought disorders
Quantitative thinking disorders
The speed of thinking is measured by the number of associations per unit of time. Highlight:
— bradylogy
(Greek bradys - slow; logos - mind) or
bradyphrenia
(Greek bradys - slow; phren - mind) -
slow thinking.
The term “bradylogy”, proposed in 1876 by A. Kussmaul, more accurately reflects the essence of the phenomenon, but is not widely used. The term “bradyphrenia” is usually used as a synonym, although more often bradyphrenia is understood as a slowdown in all mental processes;
— sperrnugi
(German sperrung - stop) - breaks in thinking;
— tachyphrenia
(Greek tachys - fast; phren - mind) or
acceleration of
Thinking disorders associated with slowing down
Bradyphrenia,
or slowing down of thinking, characterized by a slowdown in the patient’s comprehension of ongoing events, poverty of associations, and laconicism.
He answers questions after a pause; bradyllia
(Greek bradys - slow; lalia - speech), that is, slow speech, and
bradykinesia
(Greek bradys - slow; kinesis - movement) - slowness of movements, subjective feeling of memory deterioration - are pronounced.
It is necessary to distinguish between transient
and
persistent
bradyphrenia. Bradyphrenia, as a transient disorder, is observed in subdepressive and depressive states and is included as one of the main symptoms in the depressive syndrome. With pronounced asthenic syndrome, with cerebrothenia of various origins, transient inhibition of thinking also often occurs. The presence of bradyphrenia in the structure of cerebrasthenic syndrome usually leads to a deterioration in the child’s academic performance; the question often arises of educating him in an auxiliary program. Meanwhile, with an individual approach and teaching the child at his own pace, against the background of active treatment of cerebrastia, children cope quite successfully with the school curriculum [Kovalev V.V., 1985; Dobryakov I.V., 1989].
The question of dementia and the need for differential diagnosis arise, among other things, due to the fact that bradyphrenia often occurs in mental retardation as a persistent, permanent, rather than transient psychopathological feature that does not undergo any special dynamics and is resistant to therapy. In oligophrenia, as well as in other residual organic disorders of the central nervous system, persistent bradyphrenia is presented in combination with underdevelopment of abstract logical thinking, which does not happen with transient bradyphrenia. One of the variants of the asthenic form of oligophrenia, the clinical picture of which is largely determined by bradyphrenia, is called bradypsychic [MnukhinS. S, 1961; Isaev D.N., 1982].
Bradyphrenia is observed in some forms of epilepsy after seizures. At the same time, after some time the pace of thinking is restored. This does not happen in the malignant course of epilepsy: the thinking of patients becomes persistently slow and detailed, accompanied by reduced speech activity - oligophasia
(Greek oligos - small, phasis - speech).
Bradyphrenia is a common symptom of chronic intoxication in substance abusers and drug addicts.
Thinking disorders associated with stopping it
Sperrnugi -
breaks in thinking associated with stopping the associative process. Clinically manifested by sudden stops of speech, consciousness is not impaired. Patients complain about “taking away thoughts,” sometimes interpreting this in a delusional way (“thoughts are stolen by aliens”).
It is difficult to identify Sperrungs in young children. It is more common in prepubertal and pubertal age with schizophrenia.
Thought disorders associated with its acceleration
Tachyphrenia,
or
acceleration of thinking,
is characterized by the ease of associations, their superficiality, and a rapid transition from one thought to another. With a moderate acceleration of thinking, it manifests itself in the fact that the patient motorly disinhibits, becomes verbose, and the rate of speech also increases. At the same time, productivity can be maintained and actions remain meaningful. When the patient’s condition worsens, without having time to finish one thought, he jumps to another. The most pronounced acceleration of thinking is called fuga idearum (Latin fuga - running, Greek idea - concept). In this state, the patient does not have time to translate thoughts into oral speech.
Acceleration of thinking is observed in children and adolescents in hypomanic, manic states with manic-depressive psychosis, as well as in a state of intoxication, for example, with infectious delirium, with drug intoxication with amphetamines, volatile organic solvents and some other mentally active substances. Maximum pronounced acceleration (fuga idearum) is not typical for children and occurs only at older ages.
development of thinking – previous | next – thinking disorders (continued)
Content. E. G. Eidmiller. Child Psychiatry
What is thinking
Thinking is defined differently depending on the research methodology and the discipline within which it is studied. Moreover, this category has worried many thinkers for several millennia. In simple terms, thinking is the mental process of identifying patterns in the world around us based on the values and judgments that are embedded in the brain.
However, other definitions are possible. Thus, thinking can be understood as the highest stage of information processing or the process of finding connections between objects. In neuroscience, this concept refers to the creation of complex intellectual objects from simple ones. In almost all disciplines, thinking is studied as one of the highest mental functions.
In the context of psychiatric disorders, physicians are primarily interested in such aspects as operationality, motivation, as well as the ability for associative, abstract and other types of thought processes.
At the same time, thinking in schizophrenia is almost always impaired. If you carefully study the symptoms of the disease, partially described earlier, it becomes clear that most of its symptoms directly or indirectly affect the thought process or other cognitive abilities.
We will find out exactly how schizophrenia affects different aspects of thinking, primarily operational and motivational.
PsyAndNeuro.ru
Disturbances in language production and subjective changes in the thinking process are called disorder of the form of thinking (RFM) - disorder of the form
, and not
content
(as, for example, with delirium). RFM is found in a number of mental disorders: schizophrenia, recurrent depressive disorder, bipolar affective disorder, etc.
The first descriptions of RPM in the same conceptual sense in which it is used today were made by Wilhelm Griesinger (1861), Jules Séglas (1892) and Renée Masseldon (1902). Later, Emil Kraepelin, Carl Gustav Jung and, of course, Eugen Bleuler refined the descriptions of symptoms of RFM and used them to diagnose schizophrenia.
The high prevalence of RFM in schizophrenia is explained in part because it is used to establish the diagnosis of schizophrenia. New studies have shown that RFM occurs in 27-80% of patients with schizophrenia, 60% of patients with schizoaffective disorder and 53% of patients with depression. Moreover, about 6% of healthy probands show moderate RFM.
At the moment, several scales have been validated that can be used to assess RFA, including the Thought and Language Disorder (TALD) scale and the Thought, Language, and Communication Disorders (TLC) scale. Based on these scales, the scientific literature has adopted the division of RFA into positive and negative factors*.
(*in domestic schools of psychopathology, you can more often find a division of RPM regarding tempo (acceleration, deceleration, manticism (mentism)), harmony (discontinuity, incoherence, verbigeration, paragnomenon, paralogic) and purposefulness (pathological thoroughness, perseveration, reasoning, symbolism, autistic thinking ) - editor's note)
Positive RFM is best described by weakening associations, increasing the amount of speech produced (eg, logorrhea), the use of new words (neologisms), and unnatural speech phenomena (mannered speech).
Negative RFM is conceptualized as a quantitative deficit in speech and mental production (e.g., poverty of speech, slow thinking). These symptoms are usually observed in patients with chronic schizophrenia or acute depression.
Clinically important, but ignored in previous empirical studies, subjective
positive and negative RFA factors were operationalized by the TALD scale only. Using such a model of RFM factors, where positive/negative and objective/subjective symptoms are distinguished, it is possible to identify certain features for the main nosologies (Figure 1). Thus, objective positive RFM is highest during mania, and objective negative RFM is highest during schizophrenia and recurrent depressive disorder.
Rice. 1 Psychopathological assessment of RFM according to TALD
Thus, clinicians should remember that RFAs are multidimensional, and subjective RFAs should always be clarified during the clinical interview process. It is worth considering, however, that chronic positive RFM is a diagnostic marker for schizophrenia. Moreover, RFM and various language impairments are indicators of an increased risk of transition to psychosis in at-risk individuals.
From a linguistic point of view, phonology, morphology and articulation are not affected in patients with RFM, except in extremely rare, severe cases. With the strengthening of the RPF, the syntax becomes simpler. The conceptual, semantic, and pragmatic levels are most affected by patients with RFM. In schizophrenia, the understanding of speech or text may be impaired, and therefore patients do not understand the meaning of words, sentences or conversations (concretism). At the same time, positive RFA is not associated with concretism .
From a neuropsychological perspective, RFM in individuals with schizophrenia is associated with impairments in cognitive functions such as regulatory (executive) functions, attention, verbal fluency, and working memory. Positive RFM in particular correlates with impairment of regulatory functions, and negative RFM correlates with deficits in working verbal memory. Most studies on verbal fluency report significant correlations of negative RFA with semantic and phonological verbal fluency.
High-quality meta- and mega-analyses of structural MRI in RFM patients diagnosed with schizophrenia demonstrate gray matter reduction in the left superior temporal gyrus, middle temporal gyrus, and frontal operculum (see Figure 2). These volume reductions are associated with Wernicke's and Broca's areas and are therefore likely related to neurodevelopmental development and, in particular, genetic abnormalities.
Rice. 2 Brain areas involved in RFM
The anterior dentate gyrus is shown in blue, the dorsolateral prefrontal cortex is shown in green, the superior temporal gyri is shown in red, and the middle temporal gyri is shown in yellow. Positive RFM is accompanied by a decrease in cortical volume in the left superior temporal gyrus, middle temporal gyrus, and frontal operculum. Functional MRI studies show additional involvement of the right superior temporal gyrus, middle temporal gyrus, and anterior cingulate gyrus. Negative RFM is associated with bilateral volume reductions in the medial frontal and orbitofrontal cortices.
The authors of the review also presented a model of the pathogenesis of positive RFM (Fig. 3)
Rice. 3 Pathogenesis of positive RFM
Risk genes (Dysbindin1, NRG1, G72) involved in the glutamatergic system lead to dysfunctional glutamatergic neurotransmission in the superior temporal gyrus. This effect is manifested by a decrease in volume in the left superior temporal gyrus of patients with schizophrenia who have a positive RFM, which leads to neural deactivation during speech production (in Wernicke's area). This pathogenetic model involves environmental influences such as neurodevelopmental disorders, child abuse, migration, advanced paternal age, and cannabis use, which lead to neuropsychological deficits.
The material was prepared as part of the ProSchizophrenia - a specialized section of the official website of the Russian Society of Psychiatrists, dedicated to schizophrenia, modern approaches to its diagnosis and treatment.
Prepared by: Kasyanov E.D.
Source: Kircher T. et al. Formal thought disorders: from phenomenology to neurobiology. Lancet Psychiatry. 2018 Jun;5(6):515-526. doi: 10.1016/S2215-0366(18)30059-2.
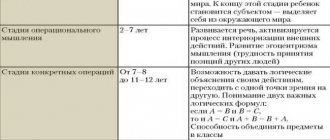
Operational aspect
Operational thinking is the ability to generalize available judgments. When analyzing this criterion, the following parameters are taken into account:
- reduction in the level of generalization;
- distortions in the generalization process;
- weakening of the categorical structure of thinking.
Let's analyze each indicator separately.
Reducing the level of generalization
If the first sign is present, a person cannot compare objects with each other, analyze the situation and generalize the information received, working with complex terms. He simply operates with general features, being unable to identify something important or specific in order to fully reveal the content of the concept.
For schizophrenics, a decrease in the level of generalization is not typical, especially at the early stage of development of schizophrenia. Typically, such symptoms are typical for patients with an oligophrenic type of disorder or patients taking antipsychotics, which are reflected in the operational side of thinking.
To obtain such indicators, simple techniques are used:
- "Classification of objects." A person is given a group of cards and asked to distribute them according to certain characteristics.
In severe cases, the patient cannot master the instructions for the task. In lighter ones, it forms classes based on uncharacteristic properties - elongated, yellow or starting with the letter “m”. In such generalizations there is no clear pattern that would reveal the true content of concepts. Thus, a subject may group scissors, a coil, and a tube into one class on the basis that all of these objects have holes. He cannot give a name to the formed group.
- "Exclusion of items." The patient excludes objects from the class based on unimportant criteria (“there is no glass here”). As a result, he copes only with very simple tasks, when an animal must be excluded from four cards on which three plants and one cat are depicted. As in the first case, there are problems with the names of the groups.
- "Pictograms". The patient is offered a list of words that he must remember. At the same time, he needs to draw something on paper that will help him correctly reproduce the resulting list. With schizophrenia, patients demonstrate specifics with personal experience, for example, “I came home from work, undressed, put the kettle on, lay down on the sofa,” etc. In a healthy person, the drawing will be more concise.
These techniques are developed not only for schizophrenics. They can also be used to examine healthy people, including children.
Distortion of the generalization process
This symptom is observed at a later stage of schizophrenia. It is associated with the qualitative characteristics of objects and concepts. The patient can operate with complex intellectual objects, but at the same time relies on their latent properties. This means that they are inherent in the phenomenon, but are not directly related to its content.
The following method can be used as an example. The patient is given cards with images of a beetle, an airplane, a bird and a butterfly. A healthy person will focus on concepts such as “animate / inanimate”, “technology / animal”, etc. However, in schizophrenia, a patient may exclude a beetle from the group just because it is depicted on a black and white card.
One patient may show signs of generalization distortion but not show symptoms of decreased generalization.
If the “pictogram” technique is used, then the patient has difficulties with abstractions - “sadness”, “doubt”, “torment”. In such cases, the phonetic features of the terms act as latent features. As a result, the patient, in order to remember them, draws objects that are consonant with the proposed words, for example, a seal (“sadness”), a catfish (“doubt”) and a bag of flour (“flour”).
Category thinking disorder
A disorder or weakening of categorical thinking is observed in cases where there is a departure from the correct thought. This phenomenon is called slippage. In general, the patient makes correct judgments, but makes isolated errors. He formulates a chain of conclusions, but at some point he gets lost. Next, he restores the thought process and continues the reasoning, but without correcting the erroneous link.
Impaired focus of thinking and Slipping
The detailing was characteristic of F.M. Dostoevsky, and if you compare the brilliant laconicism of the prose writer A.S. Pushkin and multi-page descriptions of the feelings and experiences of Dostoevsky’s heroes, then we will receive a visible description of the phenomenon of detail. The average degree of thoroughness is the actual thoroughness of thinking, when the patient constantly, systematically, throughout the entire story gets stuck on side topics, minor details, while thinking itself becomes unproductive.
An epileptic with pronounced thoroughness of thinking is very difficult for a local psychiatrist to treat as a patient at an outpatient clinic with 15 minutes allocated to the doctor per patient. Starting to answer the question about taking the drug, he will remember both his pharmacy and the road to the pharmacy with five holes on the sidewalk and ten puddles by the porch, he will remember “the infantry and his own company, and the soldier who gave me a cigarette...”. The story of such a detailed epileptic or organic makes painful the duality of the position of the doctor, who, on the one hand, must listen carefully to the patient, and on the other, not just carry out the plan of visits, but give the other patients the opportunity to talk about their pressing troubles. The third degree of thoroughness is called the viscosity of thinking and is manifested in the inability of the patient’s thinking to maintain the main guiding goal and line of conversation, his inability to return to the main topic from secondary details. Viscosity of thinking is a fundamental phenomenon of epileptic dementia.
Violation of purposeful thinking . We have already noted one of the main features of human thinking and consciousness - its direction, intentionality. Every act of consciousness is aimed at some object or object. Purposefulness is a kind of road, a path along which thought moves from one intermediate small goal to another. At the end of the road, or rather, a more or less long section of the road, there is always a goal. The stream of consciousness, or the path of thinking, rushes towards it. I'm driving a car. The goal of my journey is my house, located on such and such a street. I choose the shortest path to the goal, save gas, make various maneuvers on the road, stopping only when necessary at traffic lights, turning when I need to avoid an insurmountable obstacle. But throughout the entire journey I keep in mind the main goal - my home.
Now imagine that a girl gets into a taxi where a young, rollicking guy works as a driver. Wanting to flirt with her, he will begin to overtake other cars to the right and left, drive onto the sidewalk, change route, rush along the embankment or along the forest. The path to the final goal will not be straight and short, but somewhat confusing and winding. This will be florid thinking.
The patient uses various metaphors in speech and thinking, quotes great people appropriately and inappropriately, recalls scientific terms and reasoning from the Bible. His thinking retains external logic, the final goal, but the path to it turns out to be long.
Motivational aspect
The motivational and personal component of thinking is one of the most important in the study of mental disorders. Thus, in almost any form of schizophrenia, especially at an early stage or before an attack, there are symptoms such as apathy and lack of initiative. Any person should be interested in his destiny. If there is no concern for the future, then there will be no motivation to do anything to achieve it.
Moreover, it is important to note that there are two aspects of apathy. The first is associated with complete insensibility, which is observed in severe patients. The second is typical for milder cases, when apathy is considered as a common lack of motivation. With the first, everything is clear without an examination, but the second type of patient is sent to experts for examination, during which three main criteria are assessed:
- diversity of judgments;
- reasoning;
- criticality violations.
Let's take a closer look at each.
Diversity of judgments
With schizophrenia, a person’s judgments become contradictory. Their thought process can proceed on different planes, while the patient does not perceive such logical contradictions as errors. This is due to the lack of a clear goal for which the conclusion is formed.
In fact, the patient has several plans to solve one problem, each of which may be completely unrelated to the other. Moreover, one of them may contradict the second, but the patient does not understand this. Often one goal is dictated by the desire to complete a task, and the second is related to personal preferences.
The following case can be cited as an example. The patient is asked to distribute the cards into groups. At first he does this correctly, explaining everything clearly and logically, since the process of generalizing judgments, in principle, works well. Then he changes his mind and excludes mushrooms from the group on the basis that he was once poisoned by them and therefore does not eat them anymore.
In this case, there is a lack of goal setting. In everyday life, this will interfere with decision-making. As a result, a person may refuse to perform certain actions altogether.
A particular example of the diversity of thinking is its fragmentation, when the patient’s speech turns into a “word salad.” The beginning of a phrase refers to one situation, the middle to another, and the end to a third. In mild forms of schizophrenia, the patient may temporarily wander away from the topic due to various associations. However, he is still able to return to the topic, especially with support from a specialist.
Based on one conversation with a person, it is impossible to draw a conclusion about the fragmentation or diversity of thinking. It is necessary to carry out various techniques, including “classification” and “exclusion of items”. If contradictions appear when performing most of the tasks, appropriate conclusions are drawn about thinking disorders.
Reasoning
Reasoning is typical idle talk, a tendency to meaningless reasoning, fruitless philosophizing, which does not lead to the formation of a full-fledged intellectual product. This phenomenon is typical not only for sick people, but also for healthy people.
As an example, we can mention a student’s uncertain answer in an exam, when he does not know how to fill in his lack of knowledge of a particular subject. In such cases, he simply talks about what comes to mind, just so as not to remain silent. In general, this is an adequate human reaction to a complex and unpredictable situation. In a sense, he's just buying time.
In schizophrenia, idle talk occurs without any purpose, out of nowhere. In this case, the patient usually speaks pretentiously, pretentiously or mannered, trying to impress. He can speak with a smart look and complete platitudes that do not require any philosophizing. He does not listen to the opinions of other people at such moments. It is simply important for him to speak, especially on topics that are directly related to him. As a result, the speech turns into a long and lengthy monologue that has no clear content.
Criticality Violations
Uncriticality is characterized by a loss of purposefulness of thinking, its incompleteness. The thought process ceases to be a regulator that limits and controls a person’s actions.
To assess criticality, a simple test, or Ebbinghaus test, is performed. The patient is offered a text with gaps that he must fill in with words. He selects concepts himself, based on subjective opinion. However, in the end he must prepare a logically coherent and understandable text.
Then the expert reads it. If contradictions are detected, he asks the patient to find and correct them himself. Then the error correction rate begins to be assessed. If the subject does not see the errors, the experimenter points them out, but the patient must still make corrections on his own.
Experts distinguish three types of criticality:
- to the presence of a disease or specific symptoms;
- personal;
- to the effectiveness of their activities during experiments.
The last type of criticality is directly related to thinking. The doctor points out mistakes, and the patient corrects them. A healthy person should be interested in this, since he has a goal and his fate is important to him. A schizophrenic is usually indifferent to comments. If he was told that he did something wrong, he will accept it and do nothing. In other words, he doesn’t care - “whether it’s will or not.”
The described complex of symptoms of thinking damage is not observed in all patients. It all depends on the specific form of pathology and its stage.
Schizophrenia affects not only thinking, but also other cognitive abilities of a person - perception, attention and memory. Let's touch on them, since they are largely related to the subject discussed in the article - the thought process.
Taxonomy of thinking disorders
Here are a few examples of how thinking disorders are systematized.
E. Bleuler proposes a classification based on various criteria. He distinguishes, firstly, thinking disorders, which are common to various painful forms. These are “general relief of mental processes” and “jump of ideas”, “melancholic difficulty in associations (inhibition)”, “painfully short associations”, “monoidism”, “confusion”, “floridity and thoroughness”. Secondly, he distinguishes between thinking disorders characteristic of specific painful forms. This group includes “associations for organic psychoses”, “schizophrenic (dream-like) association disorder”, “associations for oligophrenics”, “associations for epileptics”, “associations for hysteria”, “associations for neurasthenics” and “associations for paranoids”.
K. Jaspers, who is generally skeptical about questions of systematics, distinguishes between retarded thinking, accelerated thinking and “confusion.” He considers such disorders as perseveration, verbalization, speech confusion, incoherence in the section “disorders of speech activity in psychosis.”
A.O. Bukhanovsky, Yu.A. Kutyavin, M.E. Litvak (2000) distinguish between disorders of the content of ideas and disorders of the form of the violation. The first group of disorders consists of obsessive, overvalued and delusional phenomena. The second group consists of violations of tempo, mobility, and focused thinking. The authors also include disorders of the “grammatical structure”, that is, speech.
| | For serious thinking disorders, you can make an appointment at our clinic online or call us |
A.A. Mehrabyan’s taxonomy is presented by a list of some thinking disorders. The author distinguishes the following violations:
- excitement, acceleration of thinking,
- inhibition of thinking,
- thoroughness of thinking,
- perseveration of thinking,
- reasoning,
- autistic thinking,
- paralogical thinking,
- fragmentation and incoherence of thinking.
The clarity of this approach can, unfortunately, give rise to the illusion that there are no more problems in the psychopathology of thinking, everything has been studied and there is nothing new to add to what is already known.
Let us also dwell on the taxonomy of G.I. Kaplan and B.J. Sadok (1994); it seems to us more thorough and thoughtful than others. Prefacing it with a definition of the concept of “thinking,” the authors point out that “thinking is normal if its result is a logical system of conclusions. Parapraxia (departure from the logical train of thought, also called “Freudian slips”) is considered a manifestation of normal thinking.” From the authors’ point of view, it turns out that some forms of thinking, in particular autistic thinking, are certainly pathological. The authors further distinguish between “forms of thinking disorders” and “specific thinking disorders.”
The forms of thinking disorder are:
- mental insufficiency “in the form of not entirely adequate reactions to certain events associated with experienced grief or illness”;
- “neurosis,” that is, mental disorders in which the assessment of real events and normative behavior are not impaired, but “symptoms of the disease manifest themselves as egodystonia”;
- “psychosis,” that is, the inability to distinguish reality from fiction;
- “assessment of real events: objective assessment and judgment about the world around us”;
- “violations of formal thinking” in the form of violations of associations, neologisms and illogical constructions of thoughts;
- “illogical thinking” is characterized by erroneous conclusions or internal contradictions;
- “fantasizing (dereism)”, it does not agree “with logic or experience”;
- “autistic thinking”, it expresses “only one’s own desires”, it is also characterized by “absorption by personal, internal experiences”;
- “magical thinking” as “a form of dereistic thinking” similar to the “preoperational phase in children (Piaget)”;
- "concrete thinking" or "literal thinking", when metaphors are understood without the nuances of their meaning, "in just one dimension";
- "abstract thinking" capable of "grasping the nuances of meaning", that is, "multidimensional thinking with the ability to use metaphors and hypotheses correctly."
We will not dwell on the contradictions and inaccuracies of the authors’ text. It seems to us that it is especially important here that the authors mention the existence of different forms of thinking, as if suggesting the possibility of a violation in any of them.
The authors present specific thinking disorders as follows:
1. “neologism” , that is, new words created by the patient, often by “combining syllables taken from different syllables”;
2. “verbal hash” or “incoherent mixture of words and phrases”;
3. “thoroughness of thinking” with excessive detail and an abundance of introductory words and comments;
4. “tangentiality” or “inability to make purposeful associations,” as a result of which “the patient cannot in any way get from the beginning of thought to the desired goal”;
5. “incoherent (incoherent) thinking” or “disorganized speech ... which consists of a set of words without any logical or grammatical connection”;
6. “perseveration” or “repeated repetition of responses to previous stimuli after a new stimulus has already been presented”;
7. “condensation” or “merging of different concepts into one”;
8. “irrelevant answers” - answers that do not correspond to the content of the questions asked;
9. “redundancy of associations” or “a flow of thoughts in which they constantly shift from one subject to another, not due to a logical connection”; with significant impairment, thinking may become incoherent;
10. “derailment” , that is, “a gradual or sudden deviation in the thought process without blocking, is sometimes used as a synonym for illogical associations”;
11. “flight of thought” or “rapid, continuous verbalization or play on words” with “a shift from one idea to another” and with a tendency towards “some logical connection of these ideas into a single whole”;
12. “inarticulate sounds in thinking” , that is, “associations of words that are similar in sound, but not in meaning”; "may sometimes include rhymes and puns";
13. “blocking” or “thought deprivation”, that is, “abruptly ending a thought before it is completed”;
14. “glossolalia” or “speaking in another language,” that is, “expressing thoughts in incomprehensible words.”
The authors’ distinctions between some “specific” thinking disorders are not sufficiently clear. For example, this concerns the “tangentiality” and “redundancy” of associations.
One can also note significant differences in terminology found among different authors, as well as the tendency of some of them to equate thinking disorders and speech disorders. The description of thinking disorders is presented below in the following sequence: 1. violations of the operational side of thinking, 2. violations of the logic of thinking, 3. violations of the dynamics of thinking, 4. symptoms of dissociation of thinking, 5. violations of certain types of thinking, 6. violations of certain forms of thinking.
Back to contents
Cognitive sphere in schizophrenia
First of all, schizophrenia is reflected in the perception of the surrounding reality. Changes in this area may indicate the beginning of the development of a psychopathological process, which will subsequently affect a person’s thinking and emotionality. He begins to perceive the world too subjectively, which leads to limited judgments, unrealistic or fantastic ideas.
Changes in perception are assessed using the Rorschach test, which consists of showing the patient pictures with unusual images. The subject must say what exactly he sees on the cards. As a rule, he is shown three types of images:
- deficient - “man without a head”;
- dissociative - “flattened cat”;
- symbolic - “punishment of evil.”
Analysis of the test is quite complex. You can go through it on the Internet, but you should not draw any conclusions. Only a specialist can give a normal assessment.
Attention also has its own distinctive features in schizophrenia. It is disrupted even when the patient’s memory and high intellectual level are preserved. This indicator is studied using the Schulte test, or “switch counting,” which determines how quickly a person voluntarily or involuntarily switches from one object to another. Usually, in schizophrenia, voluntary attention suffers more. At the same time, the subject does not dwell on the indicated errors, and practically does not react to the experimenter’s reactions.
Memory in schizophrenia can suffer when motivation decreases. But this phenomenon is also quite complex. In some patients it remains completely, in others it disappears partially or completely. Sometimes the patient cannot say for sure whether a particular event occurred or not.
There is also a symptom of schizophrenia called confabulation, when the brain is filled with false memories. The current ability to remember, that is, short-term memory, is tested using tests, including the “pictogram” technique.
Schizophrenia can take years to develop. Before the first attack, a person almost always does not understand that he is sick. When he is taken to the clinic, which happens during an exacerbation of the disease, a complex of symptoms is already observed. Some of them are associated with formal thinking disorders, including meaningfulness, flexibility and criticality. The degree of brain damage is determined by the type of schizophrenia and the intensity of its development.
By what signs is this condition determined?
This pathology often manifests itself in hypomania and mania, when the patient experiences the following symptoms:
- racing thoughts;
- problems in formulating ideas;
- accelerated rate of speech;
- decreased intellectual activity, memory impairment;
- the patient’s consciousness is disturbed, he loses touch with reality, the ability to be aware of many objects around him;
- with concomitant schizophrenia, mentism develops.
In all these conditions, the patient requires urgent assistance in order to stop dangerous pathologies and negative phenomena that may follow in the near future.
If timely assistance is not provided to the patient, this threatens him with serious pathological complications. A person is deprived of the ability to clearly perceive the reality around him. He cannot show conscious and correct reactions to what is happening around him, and he ceases to control himself.
Symptoms of a thinking disorder include regression of work activity and the ability to independently care for oneself at home, all of which in the near future leads to complete social disorientation. A person cannot do without constant care; he cannot take care of himself on his own.
The consequence is a state of deep depression in a person, which can lead to destructive behavior. In most cases, the most dangerous thing is the possibility of suicidal tendencies and attempts to commit suicide.