Is depression coming back - a psychiatrist's view
Recurrence of depressive episodes is not uncommon. Psychiatrists distinguish two most common types of depressive states: reactive and endogenous.
Reactive depression
arise in response to traumatic events, and most often do not require treatment; to overcome them, psychological support (psychotherapy) and time are required.
Development of endogenous depression
determined by “internal mechanisms”: disturbances of biochemical and physiological processes in the brain. Endogenous depression must be treated; moreover, the quality and timeliness of treatment will determine whether the painful depressive state will return or not.
Repetition (return) of reactive depression is a normal phenomenon, since unpleasant, threatening and traumatic events can happen to every person during their life. In such cases, depression is a healthy mental reaction that allows the nervous system to rebuild and adapt to new living conditions.
Only a severe depressive state may require psychotherapeutic (sometimes even psychiatric) help.
Recurrence of endogenous depression is always a painful condition. In some cases, the periodic repetition of depressive episodes is inherent in the very nature of the disease.
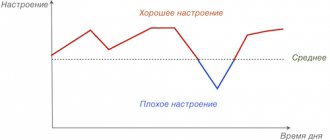
Psychiatrists distinguish a special type of “repeating” depressive episodes - recurrent depressive disorder (F 33 according to ICD-10). In such cases, the return of a depressive state is a property of the disease, due to the “weakness” of the brain structures responsible for the level of mood: after the end of depression, a so-called “bright period” of good condition may be observed, which will be replaced by a depressive state.
Who treats depression and how?
Researchers claim that even severe forms of depression and changes in brain function can be corrected. To get out of a dangerous state you will need the help of qualified specialists with knowledge of psychology, physiology and the characteristics of the body.
A psychologist
or psychotherapist
makes a diagnosis through family or individual counseling, using psychotherapeutic methods (for example, psychoanalysis or body-oriented therapy), and identifies the source of the depressive disorder.
The causes of illness in patients can be completely different, and treatment tools will be selected based on them, as well as taking into account the physical and mental state of the patient’s health.
If pharmacological treatment is necessary, antidepressants and tranquilizers are prescribed. Medicines are selected only by a psychiatrist or neurologist.
Medicines significantly improve the emotional state of patients and improve their mood. In the most severe cases, doctors may recommend hospital treatment. But here it is necessary to understand that placement in a psychiatric hospital is in itself stressful. Many people do not go to the doctor precisely because of the fear of becoming patients of such an institution. Therefore, if possible, it is better to choose a day hospital or visit doctors and strictly follow their recommendations at home. Hospitalization is only needed in cases where there is a risk of suicide and constant monitoring of the patient’s behavior becomes a necessity.
Consultation with a neurologist
It is also necessary because it will eliminate the presence of additional diseases - neuroinfections, traumatic brain injuries and others.
Visit an endocrinologist
and
a gynecologist
should be done if depression is caused by related conditions (for example, during menopause in women).
Additionally by a therapist
restorative or physiotherapeutic procedures may be prescribed.
But the most important factor in successful treatment will be the person’s desire to get rid of depressive disorder as soon as possible. But for this it is necessary not only to realize the existence of the problem, but also to put a lot of effort and patience into both the victim himself and his close circle.
What are the dangers of severe depression?
If you do nothing and do not get treatment, the main dangers of severe depression are as follows:
- A change in behavior can lead to the fact that a person simply refuses to perform everyday activities and stops taking care of himself. This can lead to lifestyle changes, exposure to dangerous communities and companies, and even suicide attempts.
- Reluctance to communicate can provoke dismissal from work, divorce, or loss of friends.
- Physical and psychological exhaustion will lead to weight loss, the occurrence of psychosomatic ailments and diseases associated with metabolic disorders.
Types of depression
Experts distinguish three types of depression based on severity: mild, moderate and severe. Severe cases can occur with or without psychotic symptoms (delusions, hallucinations, obsessive thoughts). It is necessary to be able to distinguish a difficult stage from others in order to know exactly what methods will have to be used to help a person in a difficult situation.
In a state of mild or moderate depression, the patient usually continues to go to work and communicate with people, although his quality of life is significantly reduced. In a severe form, a person is in a bad mood, does not feel interest in what is happening and does not enjoy his activities, he quickly gets tired, suffers from bouts of crying or aggression, and in some cases may even think about suicide as the only way out of this state.
Publications in the media
The brain is the main organ that responds to stress. This reaction is a complex, very complex process in which both activation and suppression of various brain structures associated with memory formation, motor, emotional and cognitive functions occur. The brain determines which situations and events may be stressful for a person, and its response to stress can be both adaptive and maladaptive (adequate or inadequate). Chronic stress leads to depression, which in turn causes damage to neural networks. Environmental stress (work stress, family stress) and especially stressful life events such as psychological trauma are the most common factors that cause depression. Since the development of new approaches to the creation of antidepressants and their use is based on a deeper understanding of the neurobiological basis of this process, it is necessary to study the influence of stress and depression at the cellular level. Depression is a chronic, recurrent, multiple etiology and life-threatening condition that consists of a set of psychological, neuroendocrine, physiological and behavioral symptoms. The severity of these symptoms determines the degree of depression, which affects up to 20% of people worldwide at some point in their lives. About 20-50% of the world's population suffers from depression, but the condition is often misdiagnosed (Wittchen, 2000). Depressive mental disorders are the most common illness in the world, causing serious socioeconomic problems (WHO, 2001). By 2015, depression is predicted to be the second leading cause of disability among Europeans after cardiovascular disease. The areas of the brain most affected by depression are the areas responsible for the formation of emotions, learning and memory, namely the prefrontal cortex, basal ganglia and hippocampus. Changes occurring in them include a decrease in the volume of structures, the size of neurons and their density, which is associated with disturbances in hemodynamics and glucose metabolism. The number of glial cells, which play a key role in transmitting nerve impulses, also decreases. The so-called “stress hypothesis” of affective mental disorders has prompted the development of animal models of depression. These models have become indispensable in preclinical studies of psychopathology, pathophysiology of depression, and specific responses to antidepressants. The discovery that the processes of neurogenesis continue in the definitive nervous system attracted great interest from the scientific community at one time, since previously the neural networks of the adult brain were considered unchanged and incapable of regeneration. This axiom was expressed in 1928 by the famous Spanish neurophysiologist Santiago Ramon y Cajal, who in one of his works wrote about nervous tissue: “here everything can die, but nothing can be restored” (Cajal, 1928). Modern research has challenged this view by demonstrating the formation of new neurons (neurogenesis) in the adult brain. In this case, the processes of neurogenesis can be enhanced by positive regulators and suppressed by negative ones, such as acute and chronic stress. While stress inhibits neurogenesis in the hippocampus, antidepressants have the opposite effect. Moreover, patients with emotional disorders on average have a hippocampus with a smaller average size than that of healthy people. When this became known, it led to the emergence of the “neurogenic hypothesis” of depression, which states that neurogenesis in the hippocampus, or rather its disturbances, may be the root cause of the development of depressive disorders. However, current thinking suggests that hippocampal neurogenesis does not play a key role in the pathogenesis of depression, although it may be responsible for some of the behavioral effects of antidepressants (Sahay & Hen, 2007). There is also growing evidence that, in addition to their effect on neurogenesis, stress and antidepressants influence the formation of specific cells of nervous tissue - glia (gliogenesis), necessary for the survival of neurons. Nerve tissue contains approximately 100 times more glial cells than neurons. Glia perform a trophic function and take part in the regulation of the transmission of nerve impulses through synapses (contacts between the processes of nerve cells). Glial cells also possess receptors for neurotransmitters and steroid hormones and are capable of generating electrical impulses. For this reason, structural changes in glial cells may be essential for the exchange of information between neurons, as well as between neurons and glia. In the adult brain, treatment with various antidepressants can stimulate not only neurogenesis, but also gliogenesis. Moreover, animal studies have shown that chronic stress suppresses cell division not only in the hippocampus but also in the prefrontal cortex, and that this effect can be reversed by antidepressants (Czeh et al., 2007). These results were confirmed by studies of patients with emotional disorders. Computed tomography has shown that the prefrontal cortex is clearly involved in pathophysiological processes. Subsequently, the condition of the tissues of deceased patients was assessed, which showed that the number of glial cells in brain samples from patients with a history of severe depression was significantly reduced. Over the past two decades, ideas about the brain have changed dramatically. It is now clear that neuronal and glial networks are not immutable, and are under the control of many factors, such as environmental factors (for example, learning), and internal factors: neurotrophins, glucocorticoids, sex hormones, etc. Antidepressants stimulate neuro- and gliogenesis, so the structural damage caused by stress and depression is not irreversible. Today it is believed that neurogenesis in the adult brain is limited to several areas: the hippocampus and areas adjacent to the lateral ventricles. However, there is increasing evidence that the formation of new neurons also occurs in the neocortex. Despite their small number, these cells are essential for the functioning of the neocortex. The relationship between mental illness and cytogenesis in the definitive neocortex is not yet clear, but preclinical studies are already underway. Perhaps, based on these works, more effective approaches to treating depression will be created. References: Wittchen HU, Hoefler M, Meister W. Depressionen in der Allgemeinpraxis. Die bundesweite Depressionsstudie. Stuttgart: Schattauer, 2000 Moussavi S, Chatterji S, Verdes E, et al. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet 2007;370:851-858 World Health Organization (WHO). The World Health Report 2001. Mental Health: New Understanding, New Hope. Download https://www.who.int/whr/2001/en/whr01_en.pdf Sahay A, Hen R. Adult hippocampal neurogenesis in depression. Nature Neuroscience 2007;10:1110-1115 Ramon y Cajal, SR. Degeneration and regeneration of the nervous system. London, Oxford University Press, 1928 Czeh B, Mueller-Keuker JIH, Rygula R, et al. Chronic social stress inhibits cell proliferation in the adult medial prefrontal cortex: hemispheric asymmetry and reversal by fluoxetine treatment. Neuropsychopharmacology 2007;32:1490-1503
Based on materials from : European College of Neuropsychopharmacology
How to assess the risk of recurrence of depression
The likelihood of a recurrence of a depressive state can be assessed by the attending physician based on the characteristics of the course of the depressive episode, its compliance (or resistance) to the therapy, and the physiological, social and psychological characteristics of the body.
For example, even such a factor as a person’s physique can play a role in the likelihood of developing (or reoccurring) depression. For example, a picnic body type is a risk factor for the return of depression.
There are no tests that reliably show the likelihood of depression recurrence. Therefore, with such a question, you should go to your doctor at the clinic, or, if this is not possible, to another psychiatrist for a consultation.
The psychiatrist's answer will most likely be in the form of a prognosis: the prognosis is favorable - the risk of recurrence is minimal, the prognosis is unfavorable - the risk is high.
Severe depression and suicide
Sometimes it happens that, being in deep depression, a person loses one of the most important instincts - the instinct of self-preservation. Melancholy and constant mental pain make him think about taking his own life. Often, terrible thoughts are also promoted by a strong feeling of guilt: a person believes that he deserves punishment, is not worthy to exist in the world, and his death will only make the life of his loved ones easier.
At the very beginning of a depressive disorder, a person is weakened and is not yet able to make such drastic decisions. But as soon as his strength returns, there is a possibility that the victim will carry out his plan, having previously created a deceptive impression among others that he is now much better.
According to psychologists, the risk group includes lonely or secluded people who suffer from psychosomatic manifestations or have a history of suicide.
It is extremely important to seek help in time and prevent the dire consequences or degeneration of depression into a chronic form.