Symptoms, age group
Childhood depression is a mental and emotional disorder whose symptoms affect behavior and physical well-being.
In children under 3 years of age, depression manifests itself in problems with appetite, frequent vomiting and regurgitation of food. There is a lack of body weight. Slowness of movements is noticeable, there is a delay in psycho-emotional development. A child with depression is whiny and capricious.
Children from 3 to 7 years old have problems with motor activity, passivity, and lack of energy. The patient strives for privacy, avoids contact even with parents. Lost interest in favorite games and activities. Facial reactions are depressed, the voice is quiet. Various fears and somatic complaints are characteristic. In younger schoolchildren, somatic symptoms dominate over mental ones.
Symptoms in children 8-11 years old:
- psychosomatics - the presence of enuresis, problems with sleep and speech communication (its suppression);
- gastrointestinal disorders, abdominal pain;
- anxiety;
- inhibition of mental activity and emotional manifestations that are noticeable in speech;
- desire for self-isolation;
- loss of interest in previously favorite games and educational process;
- difficulties in mastering the school curriculum;
- truancy;
- problems with personal hygiene;
- leaving home;
- finger sucking;
- thoughts and statements about one’s own inferiority;
- suicidal thoughts;
- sudden mood swings;
- aggressive behavior, irritability, depression.
Depression occurs earlier and more often in girls than in boys. This is likely due to the fact that girls demonstrate a higher level of sociality. For some reason, they are more dependent on social approval. The reasons for the development of pathology in girls often relate to the loss of friends or animals. The risks of the disease increase as a person gets older.
A depressed teenager: advice from a psychologist on how to avoid trouble
Parents of teenagers often pay attention to the fact that their children suddenly change: a recently cheerful child loses interest in school, friends, and life in general. He's not happy at all. The son or daughter looks tired and refuses to eat. Losing weight or, conversely, gaining weight. Many people tend to attribute this to adolescence, but it is important not to miss the onset of depression. How to recognize it and sound the alarm in time, says Elena Sizikova, family psychologist.
— What symptoms should parents be wary of?
- Sleep disturbance - insomnia or drowsiness. The child may complain of difficulty concentrating. Feelings of worthlessness and guilt (often unfounded). Sometimes depression in children manifests itself in behavior - hyperactivity, enuresis, poor performance at school. The teenager is restless, grumpy, and denies everything. Reaches to antisocial or aggressive behavior. May become sullen and avoid family contacts. Or vice versa - seem too emotional, sensitive, especially with peers. He doesn't care about his appearance or his performance at school.
- Why is this condition dangerous?
— It is often accompanied by obsessive thoughts about death, suicidal intentions or attempts. A teenager in this state may start using alcohol and drugs. Depression in a teenager should not be underestimated: it can lead to serious, dangerous, even irreparable consequences.
- How to prevent this? What to do if symptoms of depression appear?
— If you know or guess that your child is thinking about death or is a member of destructive groups on social networks, then you should urgently seek help from a psychologist. For example, to one of the family centers in Moscow. It's difficult to cope here on your own.
If we are talking about the prevention of teenage depression, then it is important to understand: adolescence is a very difficult, conflict-filled age. It is impossible to avoid conflict situations. And it's not necessary. The most important thing is to try to create such a psychological climate in the family so that the teenager feels supported, knows that he is heard and taken into account.
— It’s easy to say, but how can parents create such an atmosphere?
—
There are several methods: active emotional support for a depressed child and encouraging his positive aspirations. This will help ease the situation. It is possible and necessary to teach a teenager to socialize and overcome stress - psychologists can also help here. Another method is to expand time perspective and self-understanding.
— You said that conflicts should not be avoided, and a positive atmosphere cannot be created in a short time. How to behave correctly when conflict is inevitable?
— Communicate your fears and concerns clearly to your teen so they can understand them. Bring the teenager to a frank conversation to find out what is happening to him. He must know that he will be listened to without criticism or condemnation. An adult needs to show his willingness to listen and understand, which does not mean forgiveness. It simply creates a solid foundation on which to build further relationships. A teenager needs his parents to listen to him, but not give him advice until he asks them for it. This is difficult to come to terms with, but parents need to accept and understand: a teenager does not necessarily have to follow the advice of his elders. He makes his choice.
Only with this approach is a meaningful dialogue possible between two equal people - an adult and a teenager. Only on such a basis can constructive communication and behavior be built.
HOW TO TALK TO A TEENAGER
| If you hear | Be sure to tell me | Never say |
| “I hate studying, class...” | “What is going on here that makes you feel this way?” | “When I was your age... you’re just lazy!” |
| "Everything seems so hopeless..." | “We all feel down sometimes. Let’s think about what problems we have and which one needs to be solved first.” | “Think better about those who are worse off than you” |
| “Everyone would be better off without me!” | “You mean a lot to us, and I'm worried about your mood. Tell me what's going on" | "Do not be silly. Let's talk about something else" |
| "You do not understand me!" | “Tell me how you feel. I really want to know." | “Who can understand the youth these days?” |
| "I did a terrible thing..." | "Let's sit down and talk about it" | "What goes around comes around!" |
| “What if I don’t succeed?” | “If it doesn’t work out, I’ll know you did your best.” | “If it doesn’t work out, it means you didn’t try hard enough!” |
Source
Causes of childhood and adolescent depression
Researchers point to several possible causes or contributing factors to childhood depression:
- hereditary predisposition (often) - does not necessarily apply to first-degree relatives;
- pedagogical ignorance of parents (often) - cruel, disrespectful attitude towards the child, quarrels between mom and dad;
- social reasons (less often, rather as a triggering factor) - problems at school, parental divorce, disagreements with classmates, changes in family composition, etc.;
- psychological - emotional shock, loss of parents or death of a pet, psychological pressure from parents;
- physical or sexual abuse;
- biochemical (especially in adolescents) - problems in physical health, hormonal imbalances;
- alcoholism or drug addiction of parents, presence of mentally ill relatives;
- mild seasonal depression - the body's sensitivity to climate change.
Even in the presence of genetic determination, depression starts after some risk factors. This is often inadequate parenting, divorce, and tense relationships in the home between family members.
The second common risk factor that triggers the disease is school bullying, bullying by classmates. In this case, the child demonstrates fear or refusal to attend school.
What to do if your child is depressed
It is possible to cope with childhood depression only if parents take correct and timely action.
If you suspect your child is depressed, try the following first:
✓ talk to him. This can be difficult: teenagers, even in a normal state, are reluctant to make contact with adults, and during depression, the reluctance to share problems worsens many times over;
✓ express your support. Say that you will do your best to solve the problem. Assure of your love and willingness to help. Always be there.
The following actions:
- undergo a comprehensive diagnostics of the body;
- make an appointment with a psychotherapist and follow his instructions;
- in addition to treatment with a psychotherapist, it is worth taking a course of work with a psychologist to identify the cause of depression and prevent its recurrence;
- attend a consultation with a psychologist for parents to learn how to properly support and respond to manifestations of depression in their child.
Pathogenesis
There are biological prerequisites for the formation of the disease that can be tested in a medical setting. We are talking about a deficiency of neurotransmitters in brain synapses (norepinephrine, dopamine), and an increase in cortisol levels. Disorders of melatonin secretion are characteristic. Patients exhibit morphological changes in the amygdala and frontal cortex.
Most children with depression experience a lack of maternal love. Many experienced social and economic changes and acute stress before the onset of the disease. The disease is more often diagnosed in children who, before the disease, were already quite introverted, anxious, vulnerable and neurotic.
What else can you do
Parents always feel like they are not doing enough for their children. Especially when it comes to treating not the simplest mental disorder. Childhood depression - what else you can do for your child:
Organize your favorite activities.
During therapy, it is important to create the most comfortable home environment for the child. Due to his current difficult condition, it is worth giving up travel, noisy holidays, and lifestyle changes.
On the contrary, remember what brought joy to the child in the past. For example, singing karaoke, playing board games, cooking food together, caring for a pet. Return to these activities.
Create a space of trust.
Children make contact more easily not during a so-called confidential conversation, but in the process of some kind of joint activity. Do something with your child and talk unobtrusively. Do not ask with pressure, but simply give the opportunity to express your emotions, plans, fears. Make it a habit to communicate this way during joint activities.
Do not punish for revelations.
Inconvenient truths are hard to hear. But if you have reached a certain level of frank communication, therapy brings results, and the child decides to tell you about the not so pleasant moments in his life, do not betray his trust. Refuse the impulse to judge, subtract, punish. By these actions you will only close with a concrete wall the small door of trust that has opened in front of you.
Gradually involve your child in social interaction.
If a noisy company does not yet arouse his enthusiasm, start small. Communication with even one friend will help gradually return the child to full social interaction with others.
Bring physical activity back into your child's life.
Hiking, cycling, sports games, rollerblading or skating - any physical activity is suitable. Physical activity will not only distract you from sad thoughts, but also help relieve muscle tension.
Control your obsession with gadgets.
Being stuck on the phone itself has a negative impact on children, and during periods of depression it can become a factor slowing down recovery. It is better to leave online games and social networks for later - when the child feels better.
Watch your diet.
It has been proven that an abundance of carbohydrate foods has a negative effect on mood. Fuel your child's energy balance with healthy foods: healthy fats, quality proteins, fresh fruits and vegetables. Don't forget about healthy treats.
Give your child enough time to sleep.
If he's sleeping, don't wake him up. If he can’t sleep, turn on calm music, give him a glass of warm milk, and sit next to him. Adequate sleep is the key to rapid restoration of both physical and mental strength of the child. If you have persistent insomnia, consult your doctor about taking mild sleeping pills.
Classification
To classify depression, it is worth familiarizing yourself with the ICD-10 headings:
- F93.0 “anxiety disorder due to separation” - anxiety in relation to the person to whom the child is attached and from whom he was separated;
- F93.1 “phobic disorder” - fears that do not correspond to a certain age phase, pathological level of anxiety;
- F93.2 “social anxiety disorder” - problems in social interaction, a high level of shyness and tightness when communicating with strangers, but the absence of such indicators when interacting with family members;
- mixed variants of pathology - the presence of symptoms of all three categories.
Anxiety disorder of the first type is expressed in the child's concern about possible accidents associated with the person from whom the separation occurred. Reluctance to attend school due to fear of separation is typical. There is a fear of loneliness, nightmares about separation.
In social anxiety disorder, disruption of social interactions comes to the fore. The presence of distress and discomfort is noted in situations where the child involuntarily participates in social activities. He begins to cry, his speech is confused, and there is no spontaneous speech. Symptoms do not go away for at least 4 weeks. In this case, the disease does not progress as a gross disturbance of emotions or behavior, and there are no characteristic symptoms of PTSD or other diseases.
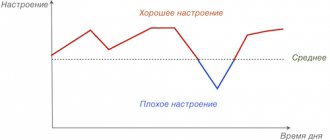
Normal or depressed state
Your child may feel sad, depressed, and cry for a while. This is a natural and extremely necessary way for our psyche to give vent to emotions.
You should not immediately run to a psychoanalyst if your child had a fight with friends or lay in bed all day. Watch!
You need to worry when symptoms of depression appear more and more often. And the child is in a normal state of mind less and less often. The line between normal and not normal is very thin.
Depressive triad
In psychotherapy, there is a symptom complex called the depressive triad - three main manifestations of depression:
- Bad mood.
- Deterioration in the quality and speed of thinking.
- Lack of motor activity (lethargy, apathy).
These three symptoms are indicators of the child's condition. If you observe kinks in one or more of them, contact a specialist.
Complications
Without medical help, childhood depression progresses into adult forms of the disorder. Symptoms worsen, new manifestations arise. Disorders increasingly affect the somatic state. During adolescence, attention should be paid to suicidal behavior. Many depressed teens demonstrate intentions to harm or kill themselves. This manifests itself in alarming moments:
- in the conversation there is a noticeable lack of hope for the future and self-confidence;
- no interest in previously favorite activities;
- indifferent attitude towards oneself or towards parents;
- gross deviations in behavior;
- preparations for suicide - writing farewell notes, wills;
- auto-aggression - self-mutilation or involvement in life-threatening activities;
- passion for the topic of death;
- straightforward statements or threatening statements about intentions to commit suicide.
The only attack of depression suffered is a huge likelihood of recurrence of the disease.
Gender differences in depression
Depression has different effects on brain activity in male and female patients in certain areas of the brain. The discovery of gender-specific effects on brain activity suggests that teenage girls and teenage boys may experience depression differently. At age 15, girls are twice as likely to be depressed as boys. There are various possible reasons for this, including problems with body image, hormonal fluctuations and genetic factors, with girls being more at risk of inheriting depression.
Differences between the sexes also influence how the disorder manifests itself and its consequences. Boys are more likely to suffer from persistent depression, while girls' depression tends to be more episodic. Compared to girls, depressed youth are also more likely to suffer the consequences of depression, such as substance abuse and suicide. But girlish depression is still more common.
Diagnostics
If you suspect depression, you should visit a psychotherapist or psychiatrist for an accurate diagnosis. Diagnosis is based not only on symptoms visible to the average person.
When diagnosing, the doctor collects information that he takes directly from the child, his parents and teachers. The patient undergoes a brief psychological test. The Beck scale, Hamilton scales and Montgomery-Asberg tests are used.
Self-diagnosis is not effective. Diagnosing a child with depression is difficult even for specialists. The reasons are that the symptoms are very variable, unstable, and masked by somatic manifestations. Children's isolation and sadness are often falsely perceived as depression. And vice versa - depression is perceived as isolation and sadness. One or three symptoms are not a sign of disease.
If a child is irritable or sad, this does not mean depression. Manifestations also depend on the characterological characteristics of the individual and age.
Depression in children
Not only a teenager, but also a much younger child can develop depression. The scientific article by M. G. Kiseleva “Depression in infants and young children” provides convincing evidence that this mental disorder can affect both a one-year-old baby and a preschooler.
The article also describes a fact confirmed by research: a child 1-5 years old is extremely dependent on the mental state of the mother. And this is what causes depression.
In 1990, an experiment was conducted: mothers were asked to maintain a “stony face” (neutral facial expressions) while communicating with their child. Those children whose mothers had experienced depression showed significantly less dissatisfaction with the “stony face” than children from the control group. This means that when the mother is depressed, the child gets used to her low involvement and passivity.
Without understanding what is happening, the child accurately reads the mother’s emotional state. And thus he himself is at risk of developing depression.
Probable Causes
Depression develops as a result of a complex interaction of biological, social and psychological factors, among which genetic predisposition, traumatic early childhood experiences and current stressful situations occupy an important place. If the first two factors are quite difficult to independently assess, then parents can pay attention to stressful situations and unfavorable events. What events can unsettle you?
1. Changes in relationships with peers, loss of a close friend for various reasons - a strong quarrel, betrayal, moving, death; ending a romantic relationship; exclusion from a significant company - the importance of the company for the teenager himself is important, while for adults, from the height of their life experience, it may seem unimportant; bullying at school (camp, social networks, etc.).
2. Sudden changes in the usual lifestyle: change of place of residence; transfer to another educational institution; unexpected illness.
3. Serious, from the teenager’s point of view, failures: low scores on the Unified State Exam or Unified State Exam; inability to enroll in the desired educational institution; failure at a competition, competition or Olympics.
4. Excessive workload and lack of time for rest and pleasant favorite activities.
5. Family influence: lack or absence of quality communication - not only about lessons, school and household responsibilities; quarrels between parents or between parents and children; adults ignoring the teenager’s feelings and psychological needs; lack of support in difficult life situations; frequent accusations, intimidation, threats, punishment - not necessarily physical; inflated expectations and demands.
6. Acute stressful situations: fire, accident, attack, violence, etc.
Effective treatment for depressive disorder
Considering the fact that in most cases the disease proceeds apathetically, and completely unusual symptoms come to the fore, we have to deal with depressive equivalents. Therefore, it is important to consult a doctor who perfectly knows the intricacies of treating the delinquent, hypochondriacal, asthenoapathic course of the disease. These are the kind of doctors who work at the Korsakov Center and are ready to provide the most competent assistance to successfully get rid of obsessive teenage depression.
We also recommend reading the article about low-grade schizophrenia.