Learn more about diseases starting with the letter “L”: Lacunar cerebral infarction, Mild cognitive impairment, Leukodystrophy, Schilder’s leukoencephalitis, Drug-induced parkinsonism, Lethargic encephalitis, Frontal syndrome, Lumbago, Lumboischialgia.
What is mild cognitive impairment
If the patient has a slight deterioration in cognitive functions compared to the state preceding the onset of the pathology, then we are talking about a cognitive disorder. The symptomatic picture of this disorder is poorly expressed. Typically, patients complain of difficulty concentrating, forgetfulness, and fatigue during mental effort. Diagnostics includes a neuropsychological or pathopsychological study of the cognitive sphere, consultation with a neurologist and psychiatrist. MCI requires an integrated approach to therapy, accompanied by the use of medications, correction of diet and daily routine, and psychocorrective exercises.
Types of cognitive thinking
Cognitive functions develop in a person from the first days of life. The child receives information about what mom smells like, what food tastes like, and how to call for help. The main stages of development are divided into three stages:
- Visually effective, it is typical for children from birth to 3 years. During this period, children collect information about the world around them using any available means: they taste, remember the smell and appearance of objects. During this period, the child distinguishes between the functions of father and mother, knows in front of whom he can make a scandal and get his way, and on whom his whims do not affect.
- Visual and figurative, it develops until the age of 7. The child learns to think logically and can now perform simple tasks, relying on previously acquired knowledge. At this age, the boundaries of what is permitted are mastered, memory is trained, and imagination develops, which parents often confuse with the desire to deceive.
- Abstract. Over 7 years old, a child already tries to imagine what cannot be touched or seen, and the ability of abstract thinking is mastered.
As children grow up, they attend various clubs and extra classes; parents strive to teach them how to play the piano, dance the waltz, speak foreign languages, and want their children to succeed in the basic program and get high scores.
But after graduating from school, it’s as if all this development ceases to matter. Children receive certificates and diplomas, become adults and are not interested in anything else. The brain stops developing, its potential sharply decreases, and along with it cognitive abilities. With age, specific terms and mathematical formulas are forgotten, and basic knowledge is erased.
Scientists have proven that if you don’t give your brain a workout every day, neural connections disintegrate, which means memory deteriorates and your ability to think decreases. Cognitive disorders appear.
General information about the disease
Translated from Latin, “cognitive” means “familiarization, cognitive.” Consequently, mild cognitive disorder (MCI) is a slight deterioration of a whole complex of intellectual abilities: concentration, memory, reproduction and processing of information, the ability to abstract and solve logical problems. However, such a disorder does not reach the level of dementia, mental retardation or amnestic syndrome. Its development is provoked by an organic or infectious disease, and MCI can occur before, during or after the underlying disease. It most often occurs in people with a low level of education. Among the patients, about 10% are elderly people over 65 years of age; it is worth noting that the majority begin to develop a symptomatic picture characteristic of Alzheimer’s within a year.
Cognitive potential in practical life
Today, many people do not read books due to wasted time on social networks and the Internet. Thus, a person does not develop cognitive abilities, and cannot achieve great heights in his skills and abilities. Thus, a person in practical life often does not know where to go to study in order to get a profession and education. Statistics show that in the CIS countries 80-90% of people do not work in their profession, and they chose the wrong educational institution. The whole problem is cognitive failure to choose the right person to become. The situation is similar with jobs. Many people work in one place for a very short period of time because the job they choose is not suitable for them. Many people often have no idea how they will succeed in life due to the fact that many become a gray mass “swimming with the flow.” The whole reason is weak cognitive potential, which does not develop for various reasons. This is just a short series where many make a mistake without realizing it. The sphere of relationships, finances, time, choice of material things, use of resources. Due to many mistakes in these important areas, a person's overall quality of life suffers.
5 most effective ways of cognitive development
We offer 5 key steps for cognitive development after reading this article.
- Discipline. This is a broad concept that manifests itself from small things to global things. How you wake up in the morning and how early you go to bed will determine your entire day. Body training and brain exercises are important every day because the body needs stress. Achieving the right goals leads you to overall success in life.
- Proper nutrition. Health is nutrition, and without health, the quality of life and development becomes dramatically more difficult. Therefore, take care of proper nutrition, drink more clean water and do not abuse bad habits. Better yet, give them up.
- Read educational literature more than social networks. Today there are many excellent materials on how to improve the quality of life by working and analyzing many areas of life. Practice and find out what can be useful to you from simple things to more complex ones.
- Develop your brain narrowly. Memory, thinking and concentration are key in brain development. The Mozgotren service is capable of effectively and most importantly quickly developing the brain at these three levels. For motivation in the service, you can track your rating and statistics.
- Get quality rest. The modern problem of humanity is the inability to rest, and this gives rise to constant fatigue and depression. Today people go on vacation, but their heads are full of business and news from the Internet. Learn to disconnect from virtual and online reality to restore strength for further achievements.
To summarize, it is worth saying that developing balanced cognition today is not difficult. It is only important to direct your time and potential in the right direction by training your brain, and not waste your energy in the wrong direction, which is suggested by various advertisements. Don't miss the opportunity to live effectively, because otherwise your life will be lived by others.
Causes
>This pathology is not a separate disease, but an intermediate state between normal and dementia. MCI is provoked by pathological processes in the central nervous system:
- Vascular diseases: multi-infarction conditions, cerebral infarctions, combined vascular and hemorrhagic brain damage, chronic cerebral ischemia. Cognitive impairment can be observed during the course of the underlying disease and as consequences;
- Neurodegenerative diseases, which include: Huntington's chorea, Parkinson's disease, senile dementia of the Alzheimer's type, progressive supranuclear palsy and dementia with Lewy bodies. Cognitive disorders precede the development of the main symptoms;
- In demyelinating pathologies, MCI manifests itself in the early stages of multiple sclerosis, progressive paralysis, and progressive multifocal leukoencephalopathy. Cognitive impairment increases as the underlying disease progresses;
- Traumatic brain injuries can cause permanent or transient cognitive impairment during the post-traumatic injury period. The clinical picture depends on the nature, depth, diffuseness or locality of the lesion;
- Dysmetabolic encephalopathies lead to metabolic disorders and dysfunction of internal organs. This provokes dysfunction of the central nervous system. Hypoglycemic, renal, disteroid, and hepatic disorders can cause cognitive impairment. Hypoxic encephalopathy, lack of protein and vitamin B, poisoning;
- If cognitive impairments are provoked by neuroinfections, then the disorder manifests itself in the early stages with Creutzfeldt-Jakob disease, HIV-associated encephalopathy, acute and subacute meningoencephalitis. In the latter case, the disorders are a consequence of the infectious process;
- With brain tumors, pathology is observed in the initial stages. Symptoms depend on the location of the tumor.
Development mechanism
The pathogenesis of the disorder is extremely diverse and depends on the underlying disease. In old age, the mechanisms of aging are decisive.
Based on cerebrovascular disorders, mild cognitive impairment develops in 68% of cases. In this case, MCI is caused by circulatory failure due to pathological changes in the cerebral vessels. The second most common condition is atrophy, that is, degenerative damage to brain tissue. About 13-15% of elderly and old patients suffer from anxiety and depressive disorders.
Diagnostic examination of patients
If you suspect a cognitive personality disorder, it is recommended to do the following:
- general clinical analysis of blood and urine;
- biochemical blood test, including electrolytes, calcium, glucose, liver and kidney function indicators, lipid spectrum;
- tests to assess the hormonal profile, levels of B vitamins and folic acid;
- CT or MRI of the brain;
- serological testing for markers of syphilis and HIV (if symptoms of the disease appear at a young or mature age);
- according to indications: ECG, chest x-ray, duplex scanning of cerebral vessels, study of cerebrospinal fluid to detect markers of Alzheimer's and dementia.
To assess the severity of the pathology, psychological testing is carried out, which consists of the following points:
- orientation in place, in time and one’s own personality: the patient is asked to name the date and place of birth, say where he is, etc.;
- a test for repeating the names of objects (sometimes it is necessary to explain their meaning), individual numbers in order or randomly;
- Praxis assessment: they are asked to perform several conscious actions, for example, fasten buttons, fold clothes;
- tests of visual-spatial perception: the patient is asked to draw simple or three-dimensional geometric figures, depict a dial and mark a certain time with arrows;
- pay attention to the peculiarities of speech, the ability to maintain a conversation;
- assessing intelligence by searching for logical associations (for example, they suggest finding something in common between a plum and an apricot).
Typical symptomatic picture
Symptoms are similar to those of cerebrospinal gravis:
If the cause of mild cognitive impairment is vascular disorders, then the onset is:
- Affective instability;
- Behavioral and emotional disorders;
- Increased anxiety;
- Fussiness and absent-mindedness.
Later, mnemonic symptoms are added. With degenerative lesions, memory problems, on the contrary, appear first.
Patients often complain of:
- Feeling of heaviness in the head;
- Headache;
- Drowsiness;
- Insomnia:
- Nausea;
- Lack of appetite;
- Dizziness;
- Intermittent sleep;
- Unsteadiness when walking.
The disturbances are not systemic; their intensity varies throughout the day, intensifying with mental and physical stress.
Possible complications
Progressive MCI without timely effective therapy can develop into dementia, which leads to the loss of self-care skills and the ability to solve everyday problems. This gives rise to problems of socialization - the circle of contacts narrows, the ability to work is lost, and the desire to attend public events disappears. With a fluctuating course, patients have difficulty performing intense mental tasks, while correct correction of the daily routine and reduction of stress allows them to maintain their usual lifestyle.
Diagnostic methods
To make a diagnosis, consultation with a psychiatrist, neurologist, or clinical psychologist is required. In this case, criteria are applied taking into account the emphasis on the state of the cognitive sphere and memory. It is necessary to distinguish between mild cognitive impairment and mental retardation, dementia and psychoorganic syndrome. For this use:
- Psychological testing, this may include pathopsychological or neuropsychological examination. There is a mild degree of impairment of short-term memory, slight instability of attention, fluctuations in dynamic mental activity. Possibly, but not necessarily, a decrease in abstract-logical function. The result is determined taking into account the patient’s level of education, age, and field of activity;
- A conversation with a psychiatrist and neurologist allows you to establish an anamnesis and identify symptoms. Characteristic complaints include general confusion, increased fatigue, difficulty concentrating and remembering. Patients working in the mental sphere note difficulty in formulating logical conclusions and abstract ideas;
- A physical examination by a neurologist is intended to establish the causes and differentiate diseases from other pathologies. Small but persistent neurological disorders may be observed: discoordination phenomena, anisoreflexia, symptoms of oral automatism and oculomotor failure. In this case, no clear syndromes can be traced.
Principles of treatment
Therapy is prescribed only after receiving the results of a diagnostic examination. But usually treatment is aimed at:
- normalization of cerebral circulation, improvement of energy metabolism in brain cells, prevention of hypoxia;
- prevention of neurodegenerative changes;
- compensation for deficiency of B vitamins and other macro- and microelements, essential amino acids;
- therapy for concomitant disorders (use of antihypertensive and antiarrhythmic drugs, hepatoprotectors, etc.).
If the cause is not eliminated, cognitive personality disorder will progress: if in a mild form of the syndrome the patient only needs help managing finances and paying for utilities, at the stage of severe dementia the patient is completely dependent on others. In such cases, we offer hospitalization in our hospital, where the person will be under round-the-clock supervision by qualified and experienced medical personnel.
You can call a doctor or make an appointment at a clinic with our operators using a 24-hour anonymous phone number 8(969)060-93-93.
Treatment for mild cognitive impairment
Treatment is designed to prevent the development of dementia, slow down the rate of cognitive impairment, and eliminate existing disorders. Treatment should be etiotropic, pathogenetic and include the use of antioxidants, antiviral neurotransmitters, vasoactive drugs, chemotherapy, surgical removal of the tumor, as well as correction of vascular disorders, depression, and dysmetabolic changes.
- Drug therapy is selected individually and includes metabolic agents and nootropics;
- Psychocorrection should be carried out regularly. This includes memorizing texts and poems, art therapy. Exercises can be carried out together with a psychologist, in a group or individually. The patient is taught to form semantic and situational connections and analyze. Monitoring the effectiveness of exercises and alternating them is necessary;
- It is also important to review your diet and daily routine. Middle-aged and older people need to reduce the amount of salt and fat they consume and increase the amount of antioxidants. It is important to maintain a daily routine that includes moderate physical activity, rational alternation of work and rest, and proper sleep. It is very important for the patient to remain socially active.
Medical prognosis
In most cases, with timely etiotropic treatment, the prognosis for most patients is positive. With a regressive course of the underlying disease, the disturbances can be reduced. Cognitive decline slows or stops.
COGNITIVE IMPAIRMENTS IN PATIENTS WITH DYSCIRCULAR ENCEPHALOPATHY IN PRACTICE
NEUROLOGIST
K.S. Zhuravleva, V.A. Kutashov
GBOU VPO VSMU im. N.N. Burdenko Ministry of Health of Russia, Department of Psychiatry and Neurology, IDPO
Russia, Voronezh
Annotation.
Chronic cerebrovascular accidents are one of the most common pathologies in medical practice. These include initial manifestations of insufficiency of blood supply to the brain (IBC) and discirculatory encephalopathy (DEP). Dyscirculatory encephalopathy (DEP) is a chronic progressive form of cerebrovascular pathology associated with multifocal or diffuse brain damage and manifested by a complex of neurological and neuropsychological disorders. At the same time, on the one hand, chronic cerebrovascular insufficiency is a risk factor for the development of stroke, and on the other hand, it is the cause of the gradual increase in various neurological and mental disorders. The social significance of this pathology is also very great, because neurological and mental
DEP disorders can cause a serious decrease in the quality of life and severe disability of patients.
Cognitive failure, which develops for various reasons in patients, is one of the most important and complex problems of modern neurology. In most countries of the world, cognitive impairment is more often associated with Alzheimer's disease than with cerebrovascular disease, and even less often with Lewy body disease and frontotemporal atrophy. However, in Russia, Finland and Asian countries (Japan, China), vascular dementia is more common than Alzheimer's disease. Moreover, in recent years there has been a tendency towards an increase in the incidence of cerebrovascular disorders not only in old age, but also among middle-aged and young people. [12].
Keywords:
dyscirculatory encephalopathy, chronic cerebrovascular accidents, cognitive impairment, vascular dementia, diagnosis, treatment.
Epidemiology of DEP.
The actual prevalence and incidence of DEP remain unknown. There is no doubt that in our country and neighboring countries there is an overdiagnosis of DEP, which is facilitated by the lack of clear, generally accepted criteria for its diagnosis. According to Western authors, moderate and severe cognitive impairment of a cerebrovascular nature, which can serve as an equivalent to DEP, is detected in 16.5% of people over 60 years of age. According to autopsy data, certain vascular changes, most often of a microvascular nature, are found in about a third of elderly people, which may correspond to the actual prevalence of DEP in this age group [3].
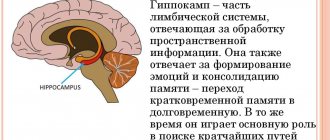
Pathogenesis of DEP:
An important role in the development of DEP is played by disruption of the functioning of neurovascular units that unite neurons, astrocytes and cells of small vessels into a single functional system. Thanks to the coupling of their activity, the phenomenon of functional hyperemia is realized: an increase in the perfusion of the activated area of the brain. This process is mediated by a number of vasoactive ions (primarily potassium and calcium), metabolic factors (carbon monoxide, hypoxia, lactate, adenosine and especially nitric oxide), neurotransmitters
(glutamate, dopamine, acetylcholine). Impaired functioning of neurovascular units leads to disruption of the mechanisms of autoregulation of cerebral circulation and disruption of the integrity of the blood-brain barrier. One of the most important links in this process is endothelial dysfunction at the level of small
cerebral vessels, causing a decrease in their reactivity and, accordingly, a deficiency in the perfusion of active areas of the brain, as well as reducing the effectiveness of traditional vasoactive drugs.
It has been shown that arterial hypertension, which is one of the main factors in the development of DEP, not only changes the structure of cerebral vessels, causing hypertrophy and remodeling of the vascular wall, promotes the development of atherosclerosis of large vessels and lipohyalinosis of small vessels, but can also block the phenomenon of functional hyperemia. This is accompanied by a decrease in the increase in perfusion in the parietal cortex and thalamus during cognitive tests, which correlates with a deterioration in their results. An increase in the permeability of the blood-brain barrier is accompanied by extravasation of plasma components both directly into the arterial wall (which contributes to its thickening and disintegration) and into adjacent areas of the brain with the development of perivascular edema (which may be one of the mechanisms of white matter damage), as well as processes of aseptic inflammation. Large areas of incomplete infarcts appear in the white matter with demyelination and loss of oligodendrocytes and axons. The main trend of pathomorphological changes in DEP is the sequential damage to the vascular wall, perivascular space and then the substance of the brain. Due to more unfavorable blood supply conditions, the subcortical and periventricular white matter of the cerebral hemispheres in DEP may suffer to a greater extent than the gray matter of the brain. Accordingly, the most universal mechanism for the development of DEP symptoms is the disconnection of cortical (primarily frontal) and subcortical structures due to damage to the pathways in the white matter of the brain. The resulting dysfunction of parallel frontal-subcortical circles, which provide both motor and mental functions, may be the direct cause of the main clinical manifestations of DEP. It should also be noted that damage to small cerebral vessels, which most often underlies DEP, can lead not only to ischemic, but also to hemorrhagic damage to the brain [1], [3].
Stages of DEP.
It is customary to distinguish 3 stages of discirculatory encephalopathy.
102
Stage I.
Complaints
for fatigue, absent-mindedness, memory impairment, especially for current events, decreased mental performance, poor general health, headaches, noise in the head, non-systemic
dizziness, emotional instability, anxious sleep.
Objectively:
scattered microsymptoms of organic damage to the nervous system - sluggish pupillary reactions, asymmetry of cranial innervation, symptoms of oral automatism, trembling of fingers of outstretched arms, etc.
Social adaptation:
Able to serve itself under normal conditions, difficulty arises only under increased load.
Stage II.
Complaints:
similar to stage I, but more pronounced, some complaints may disappear due to a decrease in criticism.
Objectively:
Severe memory disorders, including long-term memory, come to the fore, criticism of one’s state is reduced, overestimation of one’s own capabilities, excitability, verbosity are characteristic,
weakness. Intelligence begins to decline, episodes of dysarthria, impaired coordination are often observed, and pathological reflexes arise.
Social adaptation:
requires some assistance under normal conditions.
Stage III.
Complaints:
Variable, depending on the leading clinical manifestations and the safety of criticism.
Objectively:
Along with scattered symptoms, predominant damage to certain areas of the brain (subcortical nodes, brain stem, cerebellar systems, etc.) is revealed. Characteristic are amyostatic, pseudobulbar, vestibulo-cerebellar syndromes,
"vascular" dementia syndrome, drop attacks, "late" epilepsy, global amnesia syndrome.
Social adaptation:
Due to neurological and cognitive deficits, self-care is impossible and constant assistance is required [2].
Cognitive impairment in DEP. Terminology issues.
In foreign literature, the term “vascular cognitive disorders” is used to denote cognitive impairments developing as part of cerebrovascular disease.
impairment), which was proposed by V. Hachinski et al. in 1994. There are non-dementia (mild and moderate) disorders and vascular dementia.
Vascular cognitive disorders are considered the main symptom of discirculatory encephalopathy - one of the most common diagnoses in Russia, reflecting vascular suffering of the brain. The term “dyscirculatory encephalopathy” was proposed by G.A. Maksudov and V.M. Kogan in 1958 and later included in the domestic classification of lesions of the brain and spinal cord. This diagnosis exists only in domestic neurology and is not included in the International Classification of Diseases, 10th revision (ICD-10).
Cognitive impairment progresses from first to
third stage of dyscirculatory encephalopathy. Wherein
at the first and second stages, mild or moderate cognitive impairment is usually observed, and at the third stage, vascular dementia develops [4].
Vascular CIs that do not reach the level of dementia are equivalent to moderate CIs (MCI). Vascular dementia is considered as a violation of higher cortical functions, primarily regulatory, leading to social, everyday and work maladjustment. A number of authors propose to identify a group of patients with mild CI, predominantly of a neurodynamic nature. When comparing the degree of impairment of cognitive functions with the stage of DE, the initial manifestations of insufficiency of the blood supply to the brain and stage I DE correspond to the category “mild CI”, stage II DE corresponds to the “MCI” category, and stage III DE corresponds to the dementia syndrome. Progression of cognitive defect from MCI (or mild CI) to dementia within 1 year is observed in approximately 15% of patients, within 3 years - in half of the patients, and after 6 years - in 80%. Currently, the MCI criteria proposed by RS Petersen et al are used. in 1999: 1) complaints of increased forgetfulness or decreased mental performance, confirmed by the patient or his relatives; 2) information from the patient or his relatives about a decrease in cognitive functions compared to previously available capabilities; 3) objective evidence of mnestic or other CIs compared to the age norm; 4) CI should not lead to loss of professional abilities or social interaction skills, although there may be a slight deterioration in the performance of complex and instrumental types of daily and professional activities; 5) a diagnosis of dementia cannot be made. In the DSM-V classification of mental disorders, proposed in 2013, but not yet included in widespread clinical practice, there is no term “dementia” at all, but it is proposed to distinguish between minor (moderate) and major cognitive impairment. This approach, of course, shifts the emphasis of diagnosis and therapy towards the early, pre-dementia stages of intellectual-mnestic disorders [5].
Clinical picture of cognitive impairment in DEP.
The clinical picture of cognitive dysfunction in DEP is determined by the localization of lesions in various parts of the brain responsible for a certain component of cognitive activity. When changes are localized in the gray matter of the cerebral hemispheres, the cognitive defect will be of a cortical nature. However, in most cases with cerebrovascular pathology, a subcortical or cortical-subcortical variant occurs, while the neuropsychological defect is characterized by more pronounced uneven damage to executive function with better memory preservation. Along with the slowness of mental processes, rigidity of thinking, and impaired attention, patients experience secondary dysfunction of the frontal lobes of the brain, which leads to disturbances in planning, the sequence of performing certain actions, switching from one type of activity to another, and monitoring the results of activities. Ultimately, this negatively affects the performance of professional and everyday skills. It should be noted that the distinction between cognitive disorders into subcortical and cortical ones is quite arbitrary, since pathological changes in dementia affect, to one degree or another, both subcortical sections and cortical structures. Manifestations of vascular dementia rarely reach the level of deep total collapse of the psyche, characteristic of the final stages of degenerative dementias such as Alzheimer's disease or frontal dementia. The uniqueness of the clinical picture of vascular dementia also appears in combination with other psychopathological and neurological disorders. With vascular dementia, distinct neurological symptoms (pseudobulbar, extrapyramidal disorders, pelvic dysfunction, epileptic seizures) are possible at any stage of the disease, starting from the earliest.
Emotional and affective disorders are quite characteristic and varied in form at different stages of vascular brain damage. In the initial stages, they are mainly of the nature of so-called pseudoneurotic disorders and are manifested mainly by subjective symptoms. Characteristic symptoms include asthenia, fatigue, anxiety, suspiciousness, depression, emotional lability, and absent-mindedness. At the same time, criticism of his condition is completely preserved. At more pronounced stages, persistent disturbances in the emotional sphere, slowness, and rigidity of mental processes are observed. Characterological features are revealed: verbosity, viscosity, “getting stuck” on details, touchiness and quarrelsomeness, irritability, a tendency to conflict and weakness. Criticism of their condition decreases, patients stop noticing their defects and tend to overestimate themselves. Subsequently, behavioral disorders appear that have a significant impact on the patient’s quality of life.
Cognitive impairments in DEP, in addition to intellectual-mnestic disorders themselves, are also characterized by various movement disorders in the form of atactic, pseudobulbar, pyramidal and extrapyramidal disorders, indicating the separation of the frontal parts of the cerebral cortex and subcortical nuclei. Often, severe walking disorders associated with frontal ataxia (gait apraxia), pelvic disorders, as well as emotional and affective disorders may occur. The syndrome of vascular subcortical cognitive impairment is characterized by a decrease in the mobility of mental processes, accompanied by the development of bradyphrenia, as well as so-called dysregulatory disorders in the form of impaired initiation of mental activity, inertia and impulsiveness of mental processes; characterized by fluctuations in the severity of cognitive impairment throughout the day or from day to day[6].
Criteria for diagnosing cognitive impairment in DEP.
Criteria for dementia (ICD-10):
1. Progressive multiple disorders with the following manifestations:
- memory impairment (the ability to assimilate new information and reproduce previously acquired information);
- one or more of the following cognitive impairments: apraxia, aphasia, agnosia, impaired ability to synthesize, abstract, or act.
2. Cognitive impairments must cause significant difficulties in social and work adaptation.
3. Data from the anamnesis and physical examination indicate organic brain damage.
4. The cognitive defect is not associated with delirium (i.e., it develops against the background of clear consciousness).
Decreases in memory and other cognitive functions should be observed for at least 6 months.
To establish a diagnosis of vascular dementia, the following criteria must be met:
- dementia;
— heterogeneous (disproportionate) cognitive defect (some cognitive areas can be significantly impaired, others are intact);
- focal neurological symptoms (at least one of the following manifestations: central hemiparesis, unilateral increase in deep reflexes, pathological foot reflexes, pseudobulbar palsy);
- anamnestic, clinical or paraclinical signs of severe cerebrovascular disease that can cause dementia (history of stroke, signs of cerebral infarction according to computer X-ray or magnetic resonance imaging);
head tomography).
According to the criteria of the National Institute of Neurological Disorders and Stroke and the International Association for Research and Education in Neuroscience (National Institute of Neurological Disorders
and Stroke – Association Internationale pour la Recherche et l'Enseignement en Neurosciences – NINDS-AIREN), the diagnosis of vascular dementia is established
in the presence of:
1) dementia;
2) clinical, anamnestic or neuroimaging signs of cerebrovascular disease (previous strokes, transient ischemic attacks or “silent” cerebral infarctions);
3) temporary connection between vascular lesions of the brain
and cognitive impairment: development of dementia in the first
three to six months after a stroke (with the exception of the subcortical variant of vascular dementia); acute manifestation of cognitive impairment or rapid deterioration of cognitive functions.
There are a number of neuroimaging criteria for vascular dementia developed by the NINDS-AIREN working group. These include, firstly, a stroke in the area of the blood supply: - the anterior cerebral artery on both sides;
- posterior cerebral artery, including paramedian thalamic infarctions, damage to the inferomedial region of the temporal lobe;
-stroke in the associative areas (parietal-temporal, temporo-occipital territory, including the angular gyrus) and areas of adjacent blood supply to the carotid arteries (superior frontal, parietal areas).
Secondly, damage to small vessels: - lacunae in the area of the basal ganglia and white matter of the frontal lobe;
- severe periventricular leukoaraiosis;
- bilateral lesion in the area of the visual thalamus.
In addition to the above radiological changes associated with dementia, include: - infarctions in the dominant hemisphere;
- bilateral hemispheric infarctions; -leukoencephalopathy, involving at least a quarter of the total volume of white matter of the brain [7].
Methods for diagnosing cognitive impairment.
Before the formation of vascular dementia, and often at the stage of mild dementia, the presence of cognitive impairment may not be obvious during routine collection of complaints and anamnesis. Caution should be exercised in the patient's assessment of his cognitive abilities, since CIs are often accompanied by
reduction of criticism. Relatives also cannot always be objective, because they do not know what doctors should pay attention to. Therefore, to objectify cognitive status when working with elderly patients suffering from cardiovascular diseases, neuropsychological testing methods should be used. The Mini-Mental Status Scale (MMS), which is widely used to identify cognitive dysfunction associated with Alzheimer's disease (AD), is less informative in cognitive impairment of vascular etiology and cannot be the method of choice. To identify vascular CIs, a series of tests to assess frontal dysfunction (BPD), a clock drawing test, and the Montreal Cognitive Function Rating Scale should be used as screening neuropsychological tests (in addition to the CSPS).
The Mini-Cog test has proven itself to be the shortest psychometric screening technique.
MINI-COG METHOD
1. Instructions
: “Repeat three words: lemon, key, ball.” Words must be pronounced as clearly and legibly as possible, at a speed of 1 word per second. After the patient has repeated all three words, he is asked
remember these words and repeat them again. It is necessary to ensure that the patient independently remembers all three words. If necessary, words are presented repeatedly (up to 5 times).
2. Instructions
: ≪Draw a round clock with numbers on the dial and hands. All numbers should be in their places, and the arrows should point to 13.45.≫ The patient must independently draw a circle, arrange the numbers and draw arrows. Hints are not allowed. The patient should also not look at a real clock on his hand or on the wall. Instead of 13.45, you can ask to set the hands at any other time.
3. Instructions
: “Now remember the three words that we learned at the beginning.” If the patient cannot remember the words on his own, you can offer a hint. For example: “You memorized some other fruit, instrument, geometric figure.”
Interpretation
: Significant difficulty drawing a clock or difficulty reproducing at least one word with a hint indicates the presence of clinically significant cognitive impairment [8], [9].
Basic principles of treatment of DEP with cognitive impairment.
When managing patients with DE, the main directions are prevention of disease progression, organized on the basis of identified pathogenetic mechanisms, and symptomatic therapy. The possibilities of pharmacological therapy for DE are extensive, but in order to select adequate therapy, it is necessary not only to ensure its pathogenetic validity, but also to select drugs that combine a sufficiently high effectiveness and good tolerability with long-term or course use.
Etiotropic therapy for DE
•
Antihypertensive therapy
•
Antiplatelet or anticoagulant therapy
•
Lipid-lowering therapy
•
Vascular surgery methods (carotid enarterectomy, carotid artery stenting)
•
Diet low in animal fats
•
Moderate physical activity
•
Quitting smoking and alcohol abuse
The choice of treatment strategy for existing vascular cognitive impairment is determined by its severity. For dementia, drugs of the first
The choice is acetylcholinesterase inhibitors (galantamine, rivastigmine, donepilzin, ipidacrine) and/or memantine. The use of these drugs has an undoubted positive effect on memory and other cognitive functions, promotes normalization of behavior, increases adaptation to everyday life and generally improves the quality of life of patients and their relatives. According to some data, the use of these drugs also helps to reduce the rate of progression of cognitive impairment. At the stage of mild and moderate cognitive impairment, priority is given to drugs that improve cerebral microcirculation and neurometabolic processes, as well as those affecting the dopaminergic and noradrenergic neurotransmitter systems (piribedil). Vasoactive drugs (vinpocetine, pentoxifylline, standard extract of ginkgo biloba, cinnarizine, nimodipine, nicergoline) are among the most frequently prescribed drugs in neurological practice in general. These drugs promote the dilation of microcirculatory vessels without causing a “stealing effect”, affect the formed elements and improve the rheological properties of blood. In addition, they have a venotonic effect and improve venous outflow from the brain. Many vascular drugs also have additional metabolic and antioxidant properties. Neurometabolic therapy is widely used for cerebrovascular insufficiency. The goal of this therapy is to stimulate reparative processes in the brain associated with the phenomenon of neuronal plasticity. In addition, metabolic drugs have a symptomatic nootropic effect. GABAergic drugs (piracetam, aminophenylbutyric acid, etc.), peptidergic drugs (Cerebrolysin, Actovegin, Cortexin), neurotransmitter precursors (choline alfoscerate), and membrane-stabilizing drugs (citicoline) have a beneficial effect on neurometabolic processes. Under experimental conditions, it has been repeatedly shown that neurometabolic drugs help increase the survival of neurons under hypoxic conditions or when modeling a neurodegenerative process. Pathogenetically justified and appropriate is the combined implementation of vasoactive and metabolic therapy. An important aspect is also that such therapy allows for not only the correction of cognitive impairment, but also primary and/or secondary prevention of stroke. When prescribing drugs in this group, it is necessary to take into account their tolerability by patients, for example, piracetam is usually well tolerated by young people, but in older people it can cause sleep disturbances, agitation and even hallucinations, so this drug should be prescribed to patients in the older age group with caution. Particularly effective is the combined use of drugs that have a synergistic effect, for example Actovegin and Ceraxon. Against the background of intravenous administration of Actovegin (1000–2000 mg every other day), Ceraxon is prescribed at a dose of 200–300 mg (2–3 ml) 2–3 times a day [10], [11].
Conclusions:
1. Discirculatory encephalopathy is one of the most common pathologies in doctor’s practice.
2. DEP is an important medical and social problem.
3. Cognitive impairments are among the fundamental ones in the clinical picture of DEP.
4. Cognitive impairment in DEP has varying degrees of severity: from mild and moderate to vascular dementia.
5. As diagnostic methods for intellectual-mnestic disorders in DEP, it is recommended to use scales and questionnaires, batteries of tests to assess cognitive functions.
6. Treatment of cognitive impairment in DEP should be comprehensive.
Literature:
1. Shmyrev V.I., Vasilyev A.S., Rudas M.S. Discirculatory encephalopathy - issues of pathogenesis, diagnosis, differential diagnosis and treatment at the present stage // Kremlin Medicine. Clinical Bulletin. 2009. No. 4. pp. 31-36.
2. Shmyrev V.I., Vasiliev A.S., Rudas M.S. , Evdokimov A.G. Management of patients with cognitive impairment of vascular origin // Kremlin Medicine. Clinical Bulletin. 2010. No. 2. pp. 101-104.
3. Levin O.S. Dyscirculatory encephalopathy: anachronism or clinical reality? // Modern therapy in psychiatry and neurology. 2012. No. 3. pp. 40-46.
4. Golovacheva V.A., Zakharov V.V. Vascular dementia: pathogenesis, diagnosis, treatment // Neurology, neuropsychiatry, psychosomatics. 2015. No. 3. pp. 6-12.
5. Lobzin V.Yu., Emelin A.Yu., Vorobyov S.V., Lupanov I.A. Modern approaches to the diagnosis, prevention and treatment of cognitive impairment in dyscirculatory encephalopathy // Neurology, neuropsychiatry, psychosomatics. 2014. No. 2. pp. 51-56.
6. Cherdak M.A., Uspenskaya O.V. Vascular dementia // Neurology, neuropsychiatry, psychosomatics. 2010. No. 1. pp. 30-36.
7. Mistyukevich D.P. Dementia of vascular origin: etiopathogenesis, clinical picture, diagnosis, treatment // Problems of health and ecology. 2012. No. 2. pp. 27-34.
8. Vakhnina N.V. Vascular cognitive impairment // Neurology, neuropsychiatry, psychosomatics. 2014. No. 1. pp. 74-79.
9. Yakovlev N.A., Abramenko Yu.V. Emotional and cognitive disorders in men and women with dyscirculatory encephalopathy // Saratov Medical Scientific Journal. 2012. Volume 8. No. 2. pp. 570-574.
10. Zakharov V.V., Savushkina I.Yu. Diagnosis and treatment of cognitive impairment in dyscirculatory encephalopathy // Russian Medical Journal. 2011. Volume 19. No. 2. pp. 108-112.
11. Firsov A.A., Smirnov A.A., Usanova T.A., Firsova S.V. Modern possibilities for the prevention and treatment of vascular cognitive impairment // Archives of Internal Medicine. 2013. No. 3. pp. 51-56.
Information about authors:
Zhuravleva Kristina Sergeevna-
intern at the Department of Psychiatry and Neurology of the Institute of Postgraduate Education of VSMU named after. N.N. Burdenko, e-mail
Kutashov
Vyacheslav Anatolyevich
- Doctor of Medical Sciences, Professor, Head of the Department of Psychiatry and Neurology of the Institute of Postgraduate Education of VSMU named after N.N. Burdenko, e-mail
KS Zhuravleva, VA Kutashov
COGNITIVE IMPAIRMENT IN PATIENTS WITH DYSCIRCULATORY ENCEPHALOPATHY IN THE PRACTICE
NEUROLOGIST
Summary :
Chronic disorders of cerebral circulation are one of the most common pathologies in clinical practice.
These include the initial manifestations of insufficient blood supply to the brain (NPNKM) and dyscirculatory encephalopathy (DEP). Discirculatory encephalopathy (DEP) is a chronic progressive form of cerebrovascular disease associated with multifocal or diffuse lesions of the brain and manifested by a complex of neurological and neuropsychological disorders. Thus, on the one hand, chronic cerebrovascular insufficiency is a risk factor for the development of stroke, and on the other by reason of the gradual increase in various neurological and psychiatric disorders. Very high social significance of this pathology, because neurological and psychiatric disorder in the DEP can be the cause of a serious decline in the quality of life and severe disability patients. Cognitive failure, which develops for various reasons in patients, is one of the most important and challenging problems in modern neurology. In most countries, cognitive disorders are often associated with Alzheimer's disease than with vascular cerebral insufficiency, and rarely with disease Taurus Levi and frontotemporal atrophy. However, in Russia, Finland and Asian countries (Japan, China) vascular dementia is more common than Alzheimer's disease. In recent years there has been a tendency to increase the occurrence of cerebrovascular disorders not only in old age, but among persons of middle and young age. [12]. Keywords
: dyscirculatory encephalopathy, chronic violations of cerebral circulation, cognitive disorders, vascular dementia, diagnosis, treatment.
References:
1. Shmyrev VI, Vasiliev AS, Rudas MS Dyscirculatory encephalopathy - pathogenesis, diagnosis, differential diagnosis and treatment at the present stage // Kremlin medicine. Clinical Bulletin. 2009. No. 4. S. 31-36. 2. Shmyrev VI, Vasiliev AS, Rudas, MS, Evdokimov AG management of patients with cognitive impairment of vascular origin // Kremlin medicine. Clinical Bulletin. 2010. No. 2. S. 101-104. 3. Levin OS Dyscirculatory encephalopathy: a clinical anachronism or reality? // Current therapy in psychiatry and neurology. 2012. No. 3. S. 40-46. 4. Golovacheva VA, Zakharov VV Vascular dementia: pathogenesis, diagnosis, treatment // Neurology, neuropsychiatry, psychosomatika. 2015. No. 3. S. 6-12. 5. Lobzin YV, Yemelin A. Yu., Vorob'ev VS, Lupanov IA current approaches to diagnosis, prevention and therapy of cognitive disorders at dyscirculatory encephalopathy // Neurology, neuropsychiatry, psychosomatika. 2014. No. 2. S. 51-56. 6. Cherdak MA, Uspenskaya OV Vascular dementia // Neurology, neuropsychiatry, psychosomatika. 2010. No. 1. S. 30-36. 7. Matukevich DP Dementia of vascular origin: etiopathogenesis, clinic, diagnostics, treatment// Problems of health and ecology. 2012. No. 2.PP. 27-34. 8. Vakhnina N. In. Vascular cognitive disorders // Neurology, neuropsychiatry, psychosomatika. 2014. No. 1. P. 74-79. 9. Yakovlev N. And., Abramenko Y. V. Emotional and cognitive disorders in women and men with dyscirculatory encephalopathy // Saratov scientific medical journal. 2012. Volume 8. No. 2.Pp. 570-574. 10. Zakharov VV, Savushkina IY Diagnosis and treatment of cognitive disorders at dyscirculatory encephalopathy // Russian medical journal. 2011. Volume 19. No. 2. P. 108-112. 11. Firsov AA, Smirnov AA, Usanova TA, Firsova SV Modern possibilities of prevention and therapy of vascular cognitive disorders // Archives of internal medicine. 2013. No. 3. S. 51-56.